English News: Is COVID-19 a Seasonal Virus Yet?
English News: Is COVID-19 a Seasonal Virus Yet?
[[{“value”:”
The most common respiratory viruses that cause flu, colds, and RSV tend to cluster in the fall and winter months. Though that means months of elevated risk for sickness, “cold and flu season” is a convenient time for public-health officials to remind people to get vaccinated and wash their hands more frequently.
Experts had hoped that COVID-19 would follow that same pattern, but so far, that’s not the case.
[time-brightcove not-tgx=”true”]
COVID-19 occurs in every season
Both flu and RSV tend to plummet to near negligible levels in spring and summer before surging again in the fall and winter. COVID-19 does not seem to fall into that same seasonal pattern.
While COVID-19 cases also peak during the winter season, they persist throughout the spring and summer at a lower but still significant level. “We do not see COVID-19 reach the same low levels as influenza and RSV during the late spring and summer,” says Andrew Pekosz, professor of molecular microbiology and immunology at Johns Hopkins Bloomberg School of Public Health. “That’s why we can’t treat this like flu, because we are not seeing it go away like we see with flu. There is going to be a risk of getting COVID-19 year-round.”
The U.S. Centers for Disease Control and Prevention (CDC) nodded to the lack of seasonality of COVID-19 when it recently updated its vaccination guidance for older people. It advised those over 65—the age group that is currently developing more severe disease and requiring hospitalization most often—to get a second dose of the latest COVID-19 vaccine in the spring, at least four months after their first shot in the fall or winter. “We’re always driven by the data, and so far it looks like COVID-19 is not going to disappear in the spring and summer like flu and RSV,” says Dr. Wilbur Chen, professor of medicine at the University of Maryland School of Medicine and a member of the CDC committee that recommended the additional vaccine dose.
But it could start acting more like a winter virus
We are at a transitional period with COVID-19 right now, Pekosz says. As people continue to rack up more infections, vaccine doses, or both, their immunity and defenses to the once-novel virus grow. That means that on a population level, the virus is finding fewer targets to infect. Even as it morphs into different variants, past infections and shots have offered protection (so far).
For most people, therefore, COVID-19 is slowly becoming more like a seasonal disease in which their risk of infection is highest during the winter months. That helps explain the CDC’s other recent decision to relax isolation guidelines for people who have COVID-19, moving away from a five-day isolation period after someone tests positive to allowing them to resume public activities 24 hours after they no longer have symptoms such as a fever. This approach is more in line with how people treat the common cold and flu.
Over time, it’s possible that COVID-19 infections could cluster in the winter, when people spend more time indoors and the virus has more opportunity to spread. The cold, dry air also encourages transmission. “If we look at other pandemics, it takes several years for a virus to settle into a seasonal pattern that resembles what we see with flu and RSV,” Pekosz says. “I think we’re moving in that direction, but we’re certainly not there yet.”
That’s why people at high risk of complications still “need tools to protect themselves better, like an additional dose of vaccine,” he says. However, “the majority of the general population can start to treat COVID-19 a little more like a seasonal infection,” he says.
“}]]
SARS-CoV-2 is not behaving like other viruses.
Uncategorized, COVID-19, healthscienceclimate
Health – TIME
SARS-CoV-2 is not behaving like other viruses.
Read moreEnglish News: What Happened When a Man Got 217 COVID-19 Vaccines
English News: What Happened When a Man Got 217 COVID-19 Vaccines
[[{“value”:”
COVID-19 vaccines have been key to controlling the pandemic, but researchers in Germany report on one man who took the vaccination message to the extreme.
The subject of the research published in Lancet Infectious Diseases is a 62-year-old man from Magdeburg, Germany who claims to have received 217 COVID-19 vaccinations within about 2.5 years. (German prosecutors confirmed he received 130 shots in nine months during an investigation into fraud; ultimately, they did not file criminal charges.)
[time-brightcove not-tgx=”true”]
It’s not clear why the man wanted so many vaccinations or how he obtained them. But after reading news reports of the man’s story, scientists at Friedrich-Alexander-Universität Erlangen-Nürnberg (FAU) became intrigued and wanted to study how the vaccinations affected his immune system. The man—who told researchers he hadn’t experienced side effects from his shots—volunteered to provide blood and saliva samples to the scientists and allowed them to mine his health records so that they could better understand what effect aggressively stimulating the immune system with a COVID-19 vaccine might have. Even during this analysis, the man requested and received an additional two COVID-19 shots, against the advice of the study researchers.
The man’s extreme vaccination history provided a unique opportunity for scientists to see whether hyper-vaccination would positively or negatively affect the immune system’s ability to respond to pathogens like viruses. “It was unclear in which direction the 200 vaccinations would go,” says Dr. Kilian Schober, the study’s lead author and group leader at the Institute for Clinical Microbiology, Immunology, and Hygiene in Erlangen at FAU. Would these shots enhance his immune response—”like we want to see with multiple vaccinations and booster shots”—or perhaps damage it?
Read More: Why Older Adults Need Another COVID-19 Shot
Schober and the team compared the man’s immune responses—measured by his blood antibody levels, the first line of defense against a virus, and T cell levels, which are responsible for the body’s longer-term response—to those of a control group of 29 people who had received three COVID-19 shots.
Based on how the immune system works, Schober and his team thought that the man’s immune response might mirror that of people with chronic infections, such as HIV or hepatitis B. In those conditions, in which the immune system is constantly stimulated, immune cells can become overwhelmed and start to mount weaker responses.
But that’s not what they found. The man’s antibody levels and a type of T cell called effector T cells were six times higher than those in the control group on average. Those high levels proved that his immune response was strong.
However, his level of memory T cells—which are responsible for remembering viruses that a person has been infected with and replenishing the immune system’s overall T-cell population—were about the same as those in the control group. “It made sense,” says Schober, since memory T cells are reactivated when the body sees the same virus again. “But it was intriguing for us to actually see it in the data.”
According to repeated negative tests for COVID-19, which the researchers confirmed by the fact that that his immune system “showed no sign that it had dealt with the virus yet,” says Schober, the man was likely never infected with SARS-CoV-2. Schober cautions, however, against assuming that his hyper-vaccinated status was responsible for protecting him.
The researchers concluded that overall, while the man’s excessive vaccination history increased his antibody levels and apparently protected him from infection, hyper-activating his immune system did not seem to have a negative effect on his ability to mount an adequate response. At the same time, his extreme measures did not seem to afford him a level of super-immunity that distinguished his response dramatically from others who followed the recommended vaccination schedule. “His immune system was neither positively nor negatively affected,” says Schober.
“}]]
The man’s hyper-stimulated immune system reacted in a surprising way.
Uncategorized, COVID-19
Health – TIME
The man’s hyper-stimulated immune system reacted in a surprising way.
Read moreEnglish News: Researchers Are Using AI to Find New Alzheimer’s Risk Factors
English News: Researchers Are Using AI to Find New Alzheimer’s Risk Factors
[[{“value”:”
Brain experts have a pretty good handle on some of the major risk factors that contribute to Alzheimer’s—from a person’s genes to their physical activity levels, how much formal education they’ve received, and how socially engaged they are.
But one promise of AI in medicine is that it can spot less obvious links that humans can’t always see. Could AI help uncover conditions linked to Alzheimer’s that have so far been overlooked?
[time-brightcove not-tgx=”true”]
To find out, Marina Sirota and her team at University of California San Francisco (UCSF) ran a machine-learning program on a database of anonymous electronic health records from patients. The AI algorithm was trained to pull out any common features shared by people who were ultimately diagnosed with Alzheimer’s over a period of seven years. The database includes clinical data, such as lab and imaging test results and diagnoses of medical conditions.
“There were some things we saw that were expected, given the knowledge that we have about Alzheimer’s, but some of things we found were novel and interesting,” says Sirota. The results were published in Nature Aging.
Heart disease, high cholesterol, and inflammatory conditions all emerged as Alzheimer’s risk factors—not surprising, since they’re known to contribute to the buildup of protein plaques in the brain. But the less expected conditions included osteoporosis in women and depression in both men and women. The researchers also saw unexpected patterns emerge closer to when people are diagnosed, such as having lower levels of vitamin D.
Sirota and Alice Tang, a medical student in bioengineering who is the lead author of the paper, stress that these factors do not always mean that a person will develop Alzheimer’s. But they could be red flags that a patient can address to potentially lower their risk. “Picking up these factors gives us clues that a diagnosis of Alzheimer’s might be coming, and things like [high cholesterol] and osteoporosis are modifiable [with treatments],” says Tang.
Whether or not treating these issues can actually lower a person’s risk of developing Alzheimer’s isn’t clear yet; the study wasn’t designed to answer that question. Sirota and her team plan to continue mining the database of health records to determine if people receiving treatments for conditions like osteoporosis or high cholesterol, for example, eventually had a lower risk of Alzheimer’s than patients who had those conditions but didn’t treat them. “We can retrospectively look at treatment data in the electronic medical records, so that’s definitely a direction forward to determine if we can leverage any existing therapies to lower risk,” says Sirota.
Tang also hunted for genetic factors associated with things like high cholesterol or osteoporosis and Alzheimer’s that could further explain the connection between these risk factors. The link between cholesterol and Alzheimer’s turns out to be related to the ApoE gene; scientists have known that a specific form of the gene, ApoE4, is associated with a higher risk of developing Alzheimer’s. Tang also identified a gene associated with both osteoporosis and Alzheimer’s that could become a new research target for a possible treatment.
The study shows the power of machine learning in helping scientists to better understand the factors driving diseases as complex as Alzheimer’s, as well as its ability to suggest potential new ways of treating them.
More From TIME
“}]]
A machine learning program identified some unexpected links to the brain disorder.
Uncategorized, healthscienceclimate
Health – TIME
A machine learning program identified some unexpected links to the brain disorder.
Read moreEnglish News: The First Over-the-Counter Birth Control Pill Is Here
English News: The First Over-the-Counter Birth Control Pill Is Here
[[{“value”:”
The first birth control pill that people can buy without a prescription, called Opill, is shipping to stores this week.
Perrigo, the Ireland-based company that makes Opill, said the pills should be available to purchase at retail pharmacies and online by the end of March. The pills are designed to be taken daily at about the same time each day, and they will be sold in one-month packs for $19.99 and three-month packs for $49.99.
[time-brightcove not-tgx=”true”]
A spokesperson for CVS, one pharmacy that will be stocking the pill, said the pills will be in more than 7,500 of its stores nationwide and will be available to order on the store’s app. People can opt for same-day delivery or pick-up in store to preserve their privacy.
The U.S. Food and Drug Administration approved the over-the-counter use of the oral contraceptive last summer in a landmark decision. Women can now walk into any pharmacy or go online to purchase the pills without medical supervision; previously, birth control pills required a prescription and had to be dispensed by a pharmacist.
Opill contains only the hormone progestin and prevents pregnancy in several different ways, including preventing the ovaries from releasing eggs and making the uterus less hospitable for fertilized eggs to implant and grow. Because progestin is active for about 24 hours, it’s important for women to take the pill every day at about the same time for it to be most effective. Under those conditions, Opill is up to 98% effective in preventing pregnancy.
There are side effects linked to the pill, including bleeding, bloating, and abdominal pain. If these are severe and persist, women should report them to their doctor. Opill is not recommended for women with a history of breast cancer or those who are also using other forms of hormonal birth control, such as an IUD, patch, or implant.
“}]]
Women will now be able to get Opill without a prescription.
Uncategorized, healthscienceclimate
Health – TIME
Women will now be able to get Opill without a prescription.
Read moreEnglish News: Trader Joe’s Soup Dumplings Recalled For Possibly Containing Plastic
English News: Trader Joe’s Soup Dumplings Recalled For Possibly Containing Plastic
[[{“value”:”
NEW YORK — More than 61,000 pounds of steamed chicken soup dumplings sold at Trader Joe’s are being recalled for possibly containing hard plastic, U.S. regulators announced Saturday.
The Agriculture Department’s Food Safety and Inspection Service noted that the now-recalled dumplings, which are produced by the California-based CJ Foods Manufacturing Beaumont Corp., may be contaminated with foreign materials—“specifically hard plastic from a permanent marker pen.”
[time-brightcove not-tgx=”true”]
The recall arrives after consumers reported finding hard plastic in the Trader Joe’s-branded products, FSIS said. To date, no related illnesses or injures have been reported.
FSIS urged consumers to check their freezers. The 6-ounce “Trader Joe’s Steamed Chicken Soup Dumplings” under recall were produced on Dec. 7, 2023—and can be identified by their side box labels with lot codes 03.07.25.C1-1 and 03.07.25.C1-2.
In an online notice about the recall, Trader Joe’s asked consumers to throw the impacted dumplings away or return them to any store location for a full refund.
A spokesperson for CJ Foods Manufacturing Beaumont Corp. told The Associated Press that the company was investigating the issue, which happened during the manufacturing process. In an emailed statement, the food maker added that “customer safety remains our No. 1 priority.”
Foreign object contamination is one of the the top reasons for food recalls in the U.S. today. Beyond plastic, metal fragments, bits of bugs and more “extraneous” materials have prompted recalls by making their way into packaged goods.
“}]]
The dumplings may be contaminated with hard plastic from a permanent marker.
Uncategorized, healthscienceclimate, wire
Health – TIME
The dumplings may be contaminated with hard plastic from a permanent marker.
Read moreEnglish News: Zyn Is the New Vaping
English News: Zyn Is the New Vaping
[[{“value”:”
Not so long ago, Juul was seen as the new Marlboro. Smoking wasn’t that cool anymore—rates had plummeted among U.S. adults and teens—but then came Juul, a sleek, addictive product with flashy advertising tactics that took off like wildfire. It soon became clear that e-cigarettes were hooking teens who otherwise wouldn’t have gone near nicotine.
[time-brightcove not-tgx=”true”]
Now, Juul is out and Zyn is in. It’s even more discreet than Juul, with no plumes of vapor. A user simply tucks a small pouch of nicotine, additives, and flavorings under their lip for up to an hour. Over that time, it releases a steady hit of nicotine—more than that in a cigarette, but delivered much more slowly. Like Juul, it contains no tobacco.
You’re not alone if you’re just hearing of Zyn, but it’s been for sale in the U.S. since 2014. Like other products that launched around that time, including Juul, it entered the market when the U.S. Food and Drug Administration (FDA) had few regulations for new tobacco and nicotine products. The agency retroactively required these brands to prove they benefit public health enough to stay on the market, and Zyn’s manufacturer has filed those applications, but the FDA hasn’t reached decisions yet.
A lack of regulatory oversight hasn’t stopped Zyn from becoming the latest product to lure people to a new and—at least seemingly—less-dangerous way to consume nicotine. “It’s a parallel world with what happened with e-cigarettes,” says Maciej Goniewicz, a nicotine and tobacco-control researcher at Roswell Park Comprehensive Cancer Center in New York.
Still, Zyn is nowhere close to as ubiquitous as Juul once was, according to the most recent available data. About 4.5% of U.S. adults vaped and 11.5% smoked in 2021, but only about 2% used smokeless tobacco products. And just 1.5% of U.S. teenagers regularly used nicotine pouches in 2022. (For context, at the height of Juul’s popularity in 2019, 27.5% of U.S. high schoolers vaped.) “It’s not an apples-to-apples comparison,” says Corey Henry, director of U.S. communications at Zyn’s parent company, Philip Morris International (PMI). “To be honest, it’s not even an apples-to-asteroids comparison.”
But oral nicotine products have picked up significant traction in recent years. The Federal Trade Commission recently reported that the category’s U.S. sales doubled from $453 million in 2020 to more than $1 billion in 2022. And Zyn’s U.S. business grew by 62% from 2022 to 2023 alone, according to an earnings report from PMI.
Zyn is also starting to go viral, which raises concerns about the product appealing to teens who might otherwise stay away from nicotine, says Dr. Robert Jackler, a tobacco advertising expert and professor emeritus at Stanford University. “The market for these pouches is rapidly growing, and it’s being driven by many attributes that would be attractive to young people in the way e-cigarettes such as Juul were,” Jackler says, including appealing flavors and advertising that makes users look attractive, active, and cool. “We’ve seen this playbook before,” he says.
There’s even a name for people who post about the pouches—Zynfluencers—prompting concern from some public-health officials and lawmakers. Senate Majority Leader Chuck Schumer recently called for a crackdown on products like Zyn, warning parents that companies “lock their sights on young kids—teenagers, and even lower—and then use the social media to hook ’em.”
Zyn does not hire influencers or use models younger than 35 in its ads, Henry says. It also bars anyone younger than 21 from accessing its website and flags social media posts that depict underage or dangerous use of Zyn to the platforms. But the company can’t “police the internet,” Henry says. Platforms including TikTok already prohibit posts that show or encourage underage drug, alcohol, or tobacco use, yet Henry says these policies don’t always catch everything.
Henry says PMI does everything required, and more, to prevent underage Zyn use. Its ads, he says, are meant to appeal to adult tobacco users looking to switch, not teenagers. The average Zyn user is 39 and previously used another tobacco or nicotine product, according to 2023 company research conducted among customers 21 and older.
Research on the safety of nicotine pouches is ongoing. But other oral products—including snus, which is similar to Zyn but contains tobacco instead of just nicotine—have been studied for decades and seem to present significantly lower risks of cancer and other diseases, relative to cigarettes. In 2019, the FDA allowed some snus products to be explicitly sold as lower-risk alternatives.
Based on what is currently known, Goniewicz, the nicotine researcher, says it’s safe to assume nicotine pouches don’t damage the lungs because users aren’t inhaling anything. Pouches also contain fewer of the cancer-causing chemicals found in traditional chewing tobacco, he says. Their biggest health risk for adult users, in his view, likely lies in nicotine’s potential to harm the cardiovascular system.
Products like these are also risky for oral health. “Anytime you park a foreign substance between your teeth and gums, you are taking a risk of dental problems,” such as cavities and gum disease, adds Jackler, who practiced for decades as an ear, nose, and throat physician.
Some researchers have raised additional concerns. One 2023 study found that oral nicotine products like Zyn contain low levels of potentially harmful substances, including ammonia and formaldehyde. And in a small 2024 study of adults who use nicotine pouches, almost all of them reported some kind of unpleasant side effect, including mouth lesions, nausea, and a sore throat or mouth. “They certainly seem to be safer than tobacco cigarettes,” says study co-author Ashley Dowd, a postdoctoral research fellow at Johns Hopkins University. “But having a general sense that they’re safe would concern me”—especially, she says, if it prompts people who don’t currently use nicotine to pick up a pouch thinking it’s harmless.
Dowd’s study also found that most pouch users continued to smoke or vape on the side. Another 2023 study found the same thing among users ages 15 to 24. Those findings suggest that some users can’t or don’t want to completely switch from smoking to using pouches—perhaps because they don’t deliver nicotine to the bloodstream rapidly enough to quell cravings, as some recent research hints. Using multiple nicotine products is concerning, Jackler says, since it can “deepen addiction and make continuing smoking more likely.”
But if people were to entirely quit cigarettes or vapes in favor of pouches, “as a physician, I would welcome that,” Jackler says. “On the other hand, I wish they never got addicted to begin with.”
“}]]
‘It’s a parallel world with what happened with e-cigarettes’
Uncategorized, healthscienceclimate
Health – TIME
‘It’s a parallel world with what happened with e-cigarettes’
Read moreEnglish News: Yogurt Can Now Claim It May Reduce the Risk of Diabetes
English News: Yogurt Can Now Claim It May Reduce the Risk of Diabetes
[[{“value”:”
Yogurt sold in the U.S. can make claims that the food may reduce the risk of type 2 diabetes, based on limited evidence, the U.S. Food and Drug Administration said Friday.
The agency agreed that there is some evidence, but not significant scientific agreement, that eating at least 2 cups of yogurt per week may reduce the chance of developing the disease that affects about 36 million Americans.
FDA has allowed qualified health claims—a claim that lacks full scientific support but is allowed as long as there are disclaimers to keep from misleading consumers—for dietary supplements since 2000 and foods since 2002. The agency had faced lawsuits that challenged the standard of requiring scientific agreement based on claims that it violated free speech guarantees.
[time-brightcove not-tgx=”true”]
Among the allowed qualified health claims: consuming some types of cocoa may reduce heart disease and cranberry juice might reduce the risk of recurrent urinary tract infections in women.
For yogurt, Danone North America, the U.S. branch of the French firm whose brands include Dannon, Activia, and Horizon Organics yogurts, requested a qualified health claim in 2018. It submitted information from studies that observed participants over time and found a link between eating yogurt and lower markers of diabetes. The FDA agreed that there “is some credible evidence” of benefit from eating yogurt as a whole food, but not because of any particular nutrient in it.
Critics said the label change is not based on gold-standard randomized controlled trials that could have proven whether yogurt reduces diabetes risk.
No single food can reduce the risk of a disease that is tied to overall diet, the advocacy group Center for Science in the Public Interest said. It also said the label change might raise the risk of diabetes by encouraging consumption of yogurt, including types that include added sugars, and mix-ins such as cookies and pretzels.
Marion Nestle, a food policy expert, said qualified health claims based on limited evidence are “ridiculous on their face.”
“Translation: If you want to believe this, go ahead, but it’s not on the basis of evidence,” she said.
“}]]
The FDA decided to grant the food a qualified health claim.
Uncategorized, healthscienceclimate, wire
Health – TIME
The FDA decided to grant the food a qualified health claim.
Read moreEnglish News: RSV Vaccine May Be Linked to a Slightly Higher Risk of Guillain-Barre Syndrome
English News: RSV Vaccine May Be Linked to a Slightly Higher Risk of Guillain-Barre Syndrome
[[{“value”:”
NEW YORK — Health officials are investigating whether there’s a link between two new RSV vaccines and cases of a rare nervous system disorder in older U.S. adults.
The inquiry is based on fewer than two dozen cases seen among more than 9.5 million vaccine recipients, health officials said Thursday. And the available information is too limited to establish whether the shots caused the illnesses, they added.
[time-brightcove not-tgx=”true”]
But the numbers are higher than expected and officials are gathering more information to determine if the vaccines are causing the problem. The data was presented at a meeting of an expert panel that provides vaccine policy advice to the Centers for Disease Control and Prevention.
Officials said they were investigating more than 20 cases of Guillain-Barre syndrome, a rare illness in which a person’s immune system damages nerve cells, causing muscle weakness and paralysis. An estimated 3,000 to 6,000 people develop GBS in the U.S. each year, and it’s more commonly seen in older people, according to the CDC.
Most people fully recover from the syndrome, but some have permanent nerve damage. Guillain-Barre can occur in people after they are infected with a virus, but in some instances cases have been linked to vaccinations.
RSV, or respiratory syncytial virus, is a common cause of cold-like symptoms but it can be dangerous for infants and the elderly.
Last year, the CDC signed off on a recommendation made by the advisory panel, aimed at Americans age 60 and older. It was for a single dose of RSV vaccine. There were two options, one made by Pfizer and the other by GSK.
The CDC said that patients should talk to their doctors about the vaccines and then decide whether to get it.
Officials were aware that instances of Guillain-Barre had been identified in clinical trials done before the shots were approved for sale, and that different systems were watching for signs of problems.
At a meeting of the expert panel on Thursday, CDC officials presented an analysis of the reports taken in by those systems.
About two-thirds of the cases occurred in people who got a version of the vaccine made by Pfizer, called Abrysvo. But officials are also doing follow-up tracking in people who got Arexvy, made by GSK.
About two cases of Guillain-Barre might be seen in every 1 million people who receive a vaccine, health officials estimate. A CDC analysis found the the GSK rate was lower than that, but 4.6 cases per million were reported in recipients of the Pfizer shot.
Data from the U.S. Food and Drug Administration also showed an above-expected number of Guillain-Barre cases being reported in RSV vaccine recipients, with more among Pfizer shot recipients.
“Taken together, these data suggest a potential increased risk” in RSV vaccine recipients 60 and older that must be explored, said Dr. Tom Shimabukuro, a CDC vaccine safety monitoring official.
Officials from GSK and Pfizer made brief statements during the meeting, noting that sorting out a safety signal is complicated.
“Pfizer is committed to the continuous monitoring and evaluation of the safety of Abrysvo” and is conducting four safety studies to look into the possibility of vaccine-related GBS, said Reema Mehta, a Pfizer vice president.
CDC officials also presented estimates that the vaccines have prevented thousands of hospitalizations and hundreds of deaths from RSV, and that current data indicates the benefits of vaccination outweigh the possible risks.
“}]]
Officials are investigating whether there’s a link between two new RSV vaccines and cases of a rare nervous system disorder in older adults.
Uncategorized, healthscienceclimate, wire
Health – TIME
Officials are investigating whether there’s a link between two new RSV vaccines and cases of a rare nervous system disorder in older adults.
Read moreEnglish News: CVS and Walgreens to Begin Offering Abortion Pills in March
English News: CVS and Walgreens to Begin Offering Abortion Pills in March
[[{“value”:”
CVS and Walgreens will begin dispensing the abortion pill mifepristone this March, the companies confirmed to TIME.
The pharmacies received a certification to offer mifepristone—which is approved by the U.S. Food and Drug Administration to terminate a pregnancy through 10 weeks of gestation, and is often used with misoprostol—to customers with a prescription in compliance with federal and state laws. The news was first reported by the New York Times.
[time-brightcove not-tgx=”true”]
Walgreens said that it will start to dispense mifepristone within a week at select locations in New York, Pennsylvania, Massachusetts, California, and Illinois. CVS will roll out the pill in Massachusetts and Rhode Island “in the weeks ahead,” CVS spokeswoman Amy Thibault told TIME over email.
“We’ve received certification to dispense mifepristone at CVS Pharmacy and plan to fill prescriptions for this medication in states where legally permissible,” Thibault wrote. “We’re working with manufacturers and suppliers to secure the medication and are not yet dispensing it in any of our pharmacies.”
CVS said that they plan to “expand to more states, “where allowed by law, on a rolling basis.” Walgreens spokesperson Marty Maloney also confirmed to TIME over email the company’s plan to offer mifepristone in a “phased rollout” to ensure the “quality, safety, and privacy for our patients, providers, and team members.”
The future of mifepristone lies in the Supreme Court, which will hear a case about restrictions on its use this spring. The Biden Administration is hoping the court overturns an appellate ruling that would limit access to the pill by mail, among other disputes. CVS and Walgreens customers will not be able to receive the pill by mail, spokespeople from the two companies confirmed to TIME.
Since before the Supreme Court overturned Roe v. Wade in 2022, abortion pills have been the most common way to end a pregnancy.
“}]]
CVS and Walgreens will begin dispensing the abortion pill mifepristone this March, the companies confirmed to TIME.
Uncategorized, News, News Desk
Health – TIME
CVS and Walgreens will begin dispensing the abortion pill mifepristone this March, the companies confirmed to TIME.
Read moreEnglish News: Norovirus Cases Are Rising. Here’s What to Know
English News: Norovirus Cases Are Rising. Here’s What to Know
[[{“value”:”
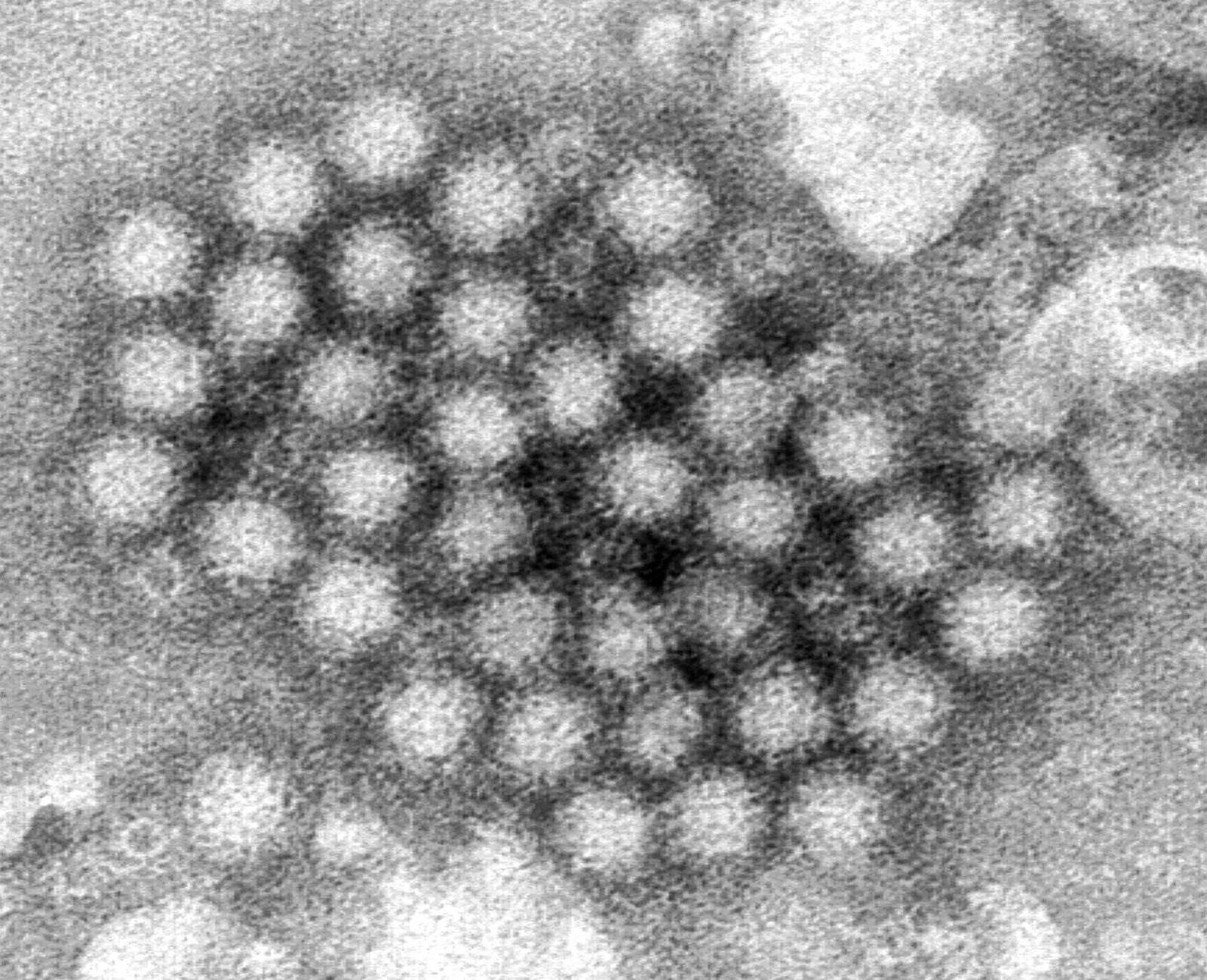
Cases of norovirus, a nasty stomach bug that spreads easily, are climbing in the Northeastern U.S., the Centers for Disease Control and Prevention reported Thursday.
Nationwide, about 12% of most recent norovirus tests sent to the CDC were positive, but the proportion was about 16% in the Northeast, the agency said. That compares with nearly 10% of norovirus tests in the Midwest and South and nearly 13% in the West.
[time-brightcove not-tgx=”true”]
Characterized by the sudden onset of vomiting, diarrhea, and general feelings of misery, norovirus outbreaks are notorious on cruise ships, nursing homes, jails, schools, and other places where people are in close contact.
Here’s what you need to know about this wily germ.
What is norovirus?
Norovirus infections are caused by a group of viruses that spread remarkably easily. It can take as few as 10 viral particles—“a miniscule amount”—to make someone sick, said Dr. William Schaffner, a infectious disease expert at Vanderbilt University Medical Center.
How does norovirus spread?
Norovirus can spread from person to person, in food or water or on contaminated surfaces. Because it’s so contagious, one handshake or a the touch of a contaminated door knob or handrail can be enough to cause illness, experts said.
How long does a norovirus illness last?
Illness caused by norovirus typically starts suddenly, in what Schaffner called “a strikingly dramatic way.” A person can go from slightly unwell to miserable within hours.
It usually lasts two to three days. Most people recover fully.
Who is at risk?
There is no medication to treat norovirus. Dehydration from vomiting and diarrhea is a chief worry, so those most at risk include young children, older people, and those with weakened immune systems.
It’s important to replace fluids by sipping water, soda, or other drinks—except coffee, tea, and alcohol—during illness, Schaffner said. Anyone experiencing symptoms of dehydration should seek medical help, he added.
How can I avoid being infected with norovirus?
The best defense against norovirus infection, especially during the peak winter season, is rigorous and frequent handwashing. Use ordinary soap and warm water and scrub hands vigorously for 20 seconds before meals.
Cleaning surfaces is important, too. Use household disinfectants and scrub well, Schaffner said.
Is this season worse than past years?
The nationwide trajectory of norovirus doesn’t seem very different this year than in past years, but there are still a few weeks left in the winter, experts noted.
The unpleasant truth is that a norovirus surge is to be expected at this time of year, said Dr. Daniel Griffin, an infectious disease expert at Columbia University Medical Center.
“We often call it ‘winter vomiting disease,’” he said.
“}]]
Cases of norovirus, a nasty stomach bug that spreads easily, are climbing in the Northeast.
Uncategorized, wire
Health – TIME
Cases of norovirus, a nasty stomach bug that spreads easily, are climbing in the Northeast.
Read moreEnglish News: The Hidden Health Costs of Climate Change
English News: The Hidden Health Costs of Climate Change
[[{“value”:”
Climate change kills. Since 2000, nearly four million people worldwide have lost their lives due to floods, wildfires, heat waves, droughts, and other extreme weather events that have been linked to a steadily warming planet, according to a recent estimate in the journal Nature. That sweeping number can make it hard for any of us to grasp how the problem is touching health in our own small part of the world. Now, a new study in Nature Medicine provides some of that granular insight for people living in the U.S., exploring how climate-linked disasters affect visits to hospital emergency departments in counties nationwide, as well as related deaths in the aftermath of the disasters. The numbers, the researchers found, are troubling, with the hardest-hit communities showing mortality rates as much as 3.8 times higher than those in surrounding areas.
[time-brightcove not-tgx=”true”]
“This could be a significant strain for hospitals and emergency departments, especially if they are damaged, lack power, or are short-staffed,” says Dr. Renee Salas, an emergency medicine physician at Massachusetts General Hospital and lead author of the study.
To conduct their work, Salas and her co-authors surveyed health records in emergency departments of major hospitals in more than 4,800 counties nationwide that had suffered billion-dollar storms—measured by property loss, insurance claims, the cost of government recovery efforts, and more—from 2011 to 2016. They focused their research on Medicare patients only, for a number of reasons. People with private insurance may pick up or lose coverage as they change jobs, making for an incomplete dataset, while Medicare coverage, once begun, is typically continued for life. What’s more, senior citizens make up the population most vulnerable to death, injury, or illness related to climate change. Finally, Medicare is taxpayer funded, and studying the health effects of climate change—and the hit on the public pocketbook that results—is important in establishing policy going forward.
“Health costs are not currently incorporated into the total economic costs of these disasters,” says Salas.
In counties that sustained the most damage from any climate-related event, emergency department use and mortality remained elevated by 1.22% and 1.4% respectively for at least one week after the event, compared to surrounding counties that suffered less damage. Those numbers may seem relatively small. But in counties for which followup data were available, the study found that those hospital visits and deaths remained elevated for up to six weeks, leading to a mortality rate 2.5 times higher than in counties that suffered less damage from the event.
Read More: Climate Change Isn’t Just a Global Threat—It’s a Public Health Emergency
Acute health problems—like smoke inhalation from wildfires, dehydration, or heat stroke from soaring temperatures—led to the greatest number of immediate visits to emergency departments or deaths. But other kinds of harm played out more slowly. Contaminated water or mold-related infections can damage health, as can loss of power that cuts off air conditioning and such essential health devices as CPAP machines. Closures of hospitals and the inability to access needed medicines may play a role too.
“People are likely to be harmed over the longer term by the things the extreme weather event caused,” says Salas. Most of the time, she adds, reports of deaths and injuries do not consider “the long tails these events appear to be having on some of the most vulnerable.”
The climate events themselves can have their own kind of long tails. Wildfires and droughts that were documented in the study tended to last about 200 to 300 days, causing elevated sickness and injury the entire time. As time goes on, those kinds of mega-crises are becoming more common. Data cited in the study and drawn from the National Centers for Environmental Information and the National Oceanic and Atmospheric Administration found that billion-dollar events account for up to 80% of all climate-related damage in the U.S. Still, the remaining 20% is not without risks. The new study, says Salas, did not provide “a complete picture of all extreme weather events.”
The world is bracing for a miserable few months when it comes to climate change. According to another study just published in Scientific Reports, a combination of greenhouse gasses and an especially intense El Niño event in the tropical Pacific Ocean will result in a 90% likelihood of record-breaking global mean surface temperatures through the end of June. The areas that are predicted to see the greatest impact are the Philippines, the Caribbean, and the Bay of Bengal region; should the heating be even worse than what the model predicts, the Amazon and Alaska will suffer acutely too. The authors of the paper warn of wildfires, cyclones, and heatwaves that will challenge the ability of local populations to adapt to or mitigate the crises—especially populations in lower income parts of the world that lack the medical infrastructure of the U.S. and other highly industrialized nations.
“Our longer-term findings are happening in a high-income country with a relatively robust health system,” says Salas. ”Death rates in low- and middle-income countries following tropical cyclones have been shown to be even greater, revealing that they may not be able to cope as well with these major climate-related disasters.”
Climate change is a planet-wide problem. It also touches the health of every one of us—nation by nation, county by county, and person by person.
“}]]
Across the U.S., billion-dollar climate events are overwhelming emergency departments.
Uncategorized, climate change, healthscienceclimate
Health – TIME
Across the U.S., billion-dollar climate events are overwhelming emergency departments.
Read moreEnglish News: Why Older Adults Need Another COVID-19 Shot
English News: Why Older Adults Need Another COVID-19 Shot
[[{“value”:”
Older adults should get the COVID-19 vaccine more frequently than previously recommended, according to new guidance from the U.S. Centers for Disease Control and Prevention (CDC). Health officials are urging people ages 65 and older to receive another vaccine dose in the spring, or at least four months after their most recent dose.
CDC director Dr. Mandy Cohen announced the decision after a CDC advisory committee, which is made up of independent vaccine and infectious disease experts, voted 11-1 to make the change. “An additional vaccine dose can provide added protection that may have decreased over time for those at highest risk,” she said in a statement.
[time-brightcove not-tgx=”true”]
The decision is based on data presented by CDC scientists that showed current hospitalization rates for COVID-19 are highest among seniors, with the biggest spikes occurring among those 75 years and older. People 65 and older account for 67% of hospitalizations due to COVID-19. (The CDC previously recommended that most people get a COVID-19 vaccine once a year. )
The committee reviewed new data showing that the current COVID-19 shot is effective against currently circulating variants including JN.1 , even though it targets XBB. People who were vaccinated with the latest shot made fewer trips to urgent care and emergency rooms for COVID-19-related symptoms, and were less likely to be hospitalized than those who did not receive the shot. But vaccine protection wanes over time, so getting another dose will help prevent serious outcomes in the most vulnerable.
Read More: Why It’s So Hard to Get Kids Vaccinated Against COVID-19
“I was convinced by the data that there is significant protection with an additional dose at this time,” says Dr. Wilbur Chen, professor of medicine at the University of Maryland School of Medicine and a member of the committee. “This recommendation isn’t for the entire population, but for high-risk segments of the population. We are trying to improve their protection as much as possible and wanted to afford those over 65 years the opportunity to get a second dose.”
One challenge to achieving that, however, is that uptake of the newest COVID-19 vaccine has been low. Though about 40% of seniors have gotten it so far—the highest rate out of any age group—it still means more than half of a very vulnerable group are not up to date. The low demand is fueling decreased access, says Chen, since more doctors’ offices are deciding not to provide the shot because their patients aren’t asking for it. Now that the government is no longer providing the vaccines for free, many people who are under- or uninsured are not getting immunized.
Chen says the committee members hope that older adults and health care providers alike receive the strong message behind the recommendation and take it seriously. “As we enter the warmer months, while we usually see flu and RSV disappear, in previous summers we still saw 500 deaths a month,” he says. “That’s a lot of deaths, and we need to act on that.”
“}]]
The CDC now recommends another dose for seniors.
Uncategorized, COVID-19, healthscienceclimate
Health – TIME
The CDC now recommends another dose for seniors.
Read moreEnglish News: Why Measles Cases Are Rising Right Now
English News: Why Measles Cases Are Rising Right Now
[[{“value”:”
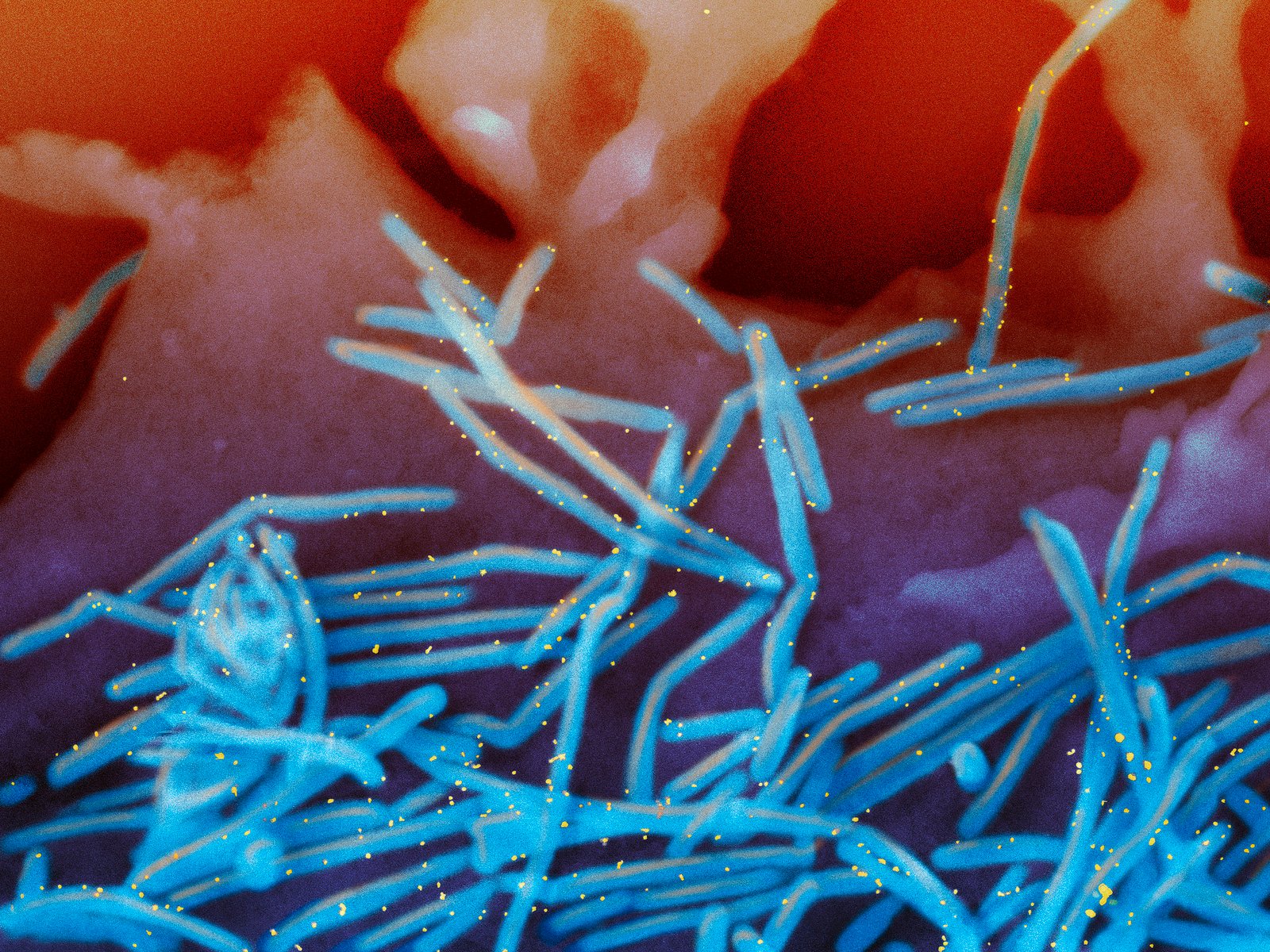
Last year, cases of measles—a serious, vaccine-preventable disease that’s highly contagious—jumped by 79% around the world. Most of them were in children. That trend is continuing this year, threatening to reverse an impressive 73% drop in measles deaths worldwide from 2000 to 2018.
Cases in the U.S. are climbing, too. In just the first two months of 2024, 35 cases have already been reported in 15 states including California, Minnesota, Florida, New York, and Louisiana; in 2023, 58 cases were reported over the entire year.
[time-brightcove not-tgx=”true”]
Why are measles cases taking off, and how can people protect themselves?
Why measles cases are climbing
Not enough kids are getting vaccinated. For herd immunity, about 95% or more of a population needs to be vaccinated, but most countries around the world have been below that threshold for years. By 2019, 86% of kids worldwide had been vaccinated with a dose by their second birthday, but that number dropped even further to 81% in 2021. (The measles vaccine is given in two doses: one at a year, the next at age 4-6.)
Vaccination rates in the U.S. are declining, too, and vaccination exemption rates are creeping up. CDC data show that 93% of kindergarteners were vaccinated against measles during the 2021-22 school year
Vaccinating more children is the best way to prevent new outbreaks. The vaccine, which has been around since the 1960s, is given as a combination shot that also includes protection against mumps and rubella. One dose is 93% effective against measles, and two doses are 97% effective. “The science really supports the safety and effectiveness of vaccinations,” says Dr. Katherine Baumgarten, medical director for infection control and prevention at Ochsner Health in New Orleans. However, “we know there is a lot of distrust in vaccines, and that’s a shame. If vaccination rates continue to decline, then we will see more of the diseases that we had hoped to completely eliminate.”
How measles spreads
Measles is one of the most contagious diseases on the planet. It spreads through the air, by infectious droplets, and on surfaces. “If a person has not been exposed or vaccinated, then they generally get infected if they are exposed 90% of the time,” Baumgarten says. Measles can cause a rash, high fevers, and even brain swelling and death.
Cases pose a particular threat to people who can’t get vaccinated, such as babies less than a year old, people who have weakened immune systems due to medical conditions or transplant surgeries, and pregnant women—even if they’ve been vaccinated—since their immune systems are more susceptible while they are expecting. “If [people with measles] come to a doctor of hospital for care and are in a waiting room with other patients, they may expose other people,” Baumgarten says.
Why fewer kids are getting vaccinated
Growing vaccine-refusal is one reason. Another is COVID-19.
Measles cases had started climbing in 2019, but they dropped significantly in 2020, when much of the world went into lockdown and adopted stricter public health prevention measures, such as wearing masks and practicing social distancing. Those behaviors make it harder for any virus, including measles, to spread. It’s also possible that following the surge in cases in 2019, more of the world’s children became immune because they had contracted the infection, and therefore fewer were susceptible to the disease.
But lockdowns also interrupted kids’ vaccinations. As health resources shifted to controlling the pandemic, vaccination programs around the world were put on hold. The World Health Organization (WHO) estimates that 22 million children missed the first dose of their measles vaccine in 2022, most likely due to disruption caused by COVID-19.
Many of those kids still aren’t immunized. Some countries have strict programs for vaccinating kids at specific ages, so if child misses their window, they may find it hard to get immunized later on. “We do have more susceptible children globally, so outbreaks could get bigger and more frequent,” says Dr. William Moss, executive director of the International Vaccine Access Center at Johns Hopkins Bloomberg School of Public Health. “For an outbreak, you need two things: a susceptible pool of people, mostly children, and introduction of the virus.”
Outbreaks tend to originate elsewhere—but experts are still worried
There doesn’t seem to be a reservoir of virus endemic to the U.S. that’s seeding new cases. Most outbreaks in various states start when a person contracts measles during travel, then returns home.
But that scenario is still concerning, especially for communities where measles vaccination coverage is lower due to growing anti-vaccine sentiment or religious reasons for avoiding immunizations. In those areas, a susceptible population plus introduction of the measles virus could spawn a cluster of cases, Moss says.
“}]]
Vaccinations are declining, and the virus is getting more chances to spread.
Uncategorized, healthscienceclimate
Health – TIME
Vaccinations are declining, and the virus is getting more chances to spread.
Read moreEnglish News: Wendy Williams Documentary Producers Say They Were Unaware of Her Dementia While Filming Most Scenes
English News: Wendy Williams Documentary Producers Say They Were Unaware of Her Dementia While Filming Most Scenes
[[{“value”:”
If you watched Lifetime’s Wendy Williams docuseries that premiered over the weekend and felt uncomfortable, you weren’t alone.
“Where is Wendy Williams?” premiered over the weekend and featured numerous scenes of the former talk show host unsteady, belligerent, confused and also drunk. Her manager would regularly find liquor bottles hidden throughout her apartment, behavior that producers say unnerved them while filming. But they say they didn’t know at the time that Williams had dementia, which the public learned late last week.
[time-brightcove not-tgx=”true”]
“We all became very concerned for her safety. To be honest, I was so concerned she would fall down the stairs and for numerous different reasons,” said Erica Hanson, an executive producer who can be seen and heard speaking to Williams at certain moments in the series.
Hanson said soon after she and the filmmakers were told Williams had dementia by her son, they turned the cameras off.
“We decided to stop filming as a team. We kept hoping that she was going to get better but it became apparent to us that she was not and that she really needed help,” Hanson said.
“Where is Wendy Williams?” debuted Saturday, two days after her care team released a statement saying she has been diagnosed with primary progressive aphasia and frontotemporal dementia, the same disease Bruce Willis has. Its two episodes aired after attorneys for Lifetime successfully fended off an effort by Williams’ guardian to stop the broadcasts.
Read More: What It’s Like Living With Aphasia—and How to Support a Loved One With the Condition
In a review, Variety called the series “an exploitive display of her cognitive decline and emotional well-being.” Danie Buchanan, a radio DJ in Atlanta posted a video reaction on Instagram saying, “I couldn’t finish it … It was so hard to watch, it was so hard to see her like that,” she said.
Throughout the documentary, Williams appears unsteady on her feet and she has trouble walking without assistance. Her emotions fluctuate between sweet to suddenly irritable to belligerent to weepy or frustrated. Many times the former talk show host admits to drinking. “I love vodka,” Williams, 59, says in the first episode.
She has been public about her cocaine addiction and lived in a “sober house” in 2019. Each time someone brings up her drinking on camera, Williams ends the conversation.
In April 2023, the film crew followed Williams to Miami to visit her son Kevin, Jr. and other family. During the trip, Williams’ son told the filmmakers that his mother suffers from a form of dementia caused by alcohol.
“We didn’t find out the diagnosis until Kevin Jr. shared that with us,” said Brie Bryant, Lifetime’s senior vice president of non-scripted programming.
Read More: State Driver’s License Laws Could Lead to Underdiagnosis of Dementia, According to New Research
After returning from Miami, the crew arrived at Williams’ apartment to find her sobbing in her bed, seemingly inebriated. This was the tipping point — Hanson was filmed speaking with Williams’ manager, Will Selby, about her condition, before they stopped filming Williams altogether. Shortly after she was placed in a treatment facility by her guardianship.
“We questioned all the time, ‘Should we be here? Should we not? How can we tell this story sensitively?’ It touched all of us deeply. It really did,” Hanson said.
The project was intended to be a follow-up to Lifetime’s 2021 “Wendy Williams: What a Mess!” documentary and biopic “Wendy Williams: The Movie.” Bryant said both the network and Williams enjoyed their partnership and agreed to film Williams’ next chapter.
The objective, said Hanson, was to document a woman making changes in her life, facing obstacles, and coming out the other side. Williams’ self-titled daytime talk show ended in 2022 because of ongoing health issues with Graves’ disease that kept her from filming. Sherri Shepherd, a guest host for Williams, was given her own show.
“We thought we were going to film a woman at a real turning point in her life, embarking on a new career with Wendy doing a podcast … recovering from a very difficult divorce,” said Hanson. “Once we started filming, it really went into a very different direction.”
Read More: Air Pollution May Be Increasing the Risk of Dementia, Study Says
Producers say ultimately what was filmed and aired is honest and unfiltered, like Williams herself.
“It is a painful truth, and it’s a very sad truth,” added executive producer Mark Ford, “but Wendy is one of the most radically honest storytellers in the history of media. Why would this documentary not echo that incredible legacy of of openness?”
Bryant says there is “no conversation” about filming more with Williams in the future. “The only thing that we care about at Lifetime is that she had a platform to tell her story, and that we feel we did so responsibly, and that she gets well and hopefully gets to be with her family.”
The filmmakers say they hope the series makes people take a closer look at guardianships. Because Williams’ finances and medical care are managed by a third party, her family says they are unable to see her and have a say in her treatment.
“We hope that people can see why we aired it, and produced it, and that the intention is to shine a light on the difficulties and the secrecies in these guardianships,” Ford said.
“}]]
“Where is Wendy Williams?” featured numerous scenes of the former talk show host unsteady, belligerent, confused and also drunk.
Uncategorized, News Desk, wire
Health – TIME
“Where is Wendy Williams?” featured numerous scenes of the former talk show host unsteady, belligerent, confused and also drunk.
Read moreEnglish News: Long COVID Doesn’t Always Look Like You Think It Does
English News: Long COVID Doesn’t Always Look Like You Think It Does
[[{“value”:”
In the spring of 2023, after her third case of COVID-19, Jennifer Robertson started to feel strange. Her heart raced all day long and she could barely sleep at night. She had dizzy spells. She felt pins and needles in her arm, she says, a “buzzing feeling” in her foot, and pain in her legs and lymph nodes. She broke out in a rash. She smelled “phantom” cigarette smoke, even when none was in the air.
[time-brightcove not-tgx=”true”]
Robertson, 48, had a feeling COVID-19 might have somehow been the trigger. She knew about Long COVID, the name for chronic symptoms following an infection, because her 11-year-old son has it. But “he didn’t have anything like this,” she says. “His set of symptoms are totally different,” involving spiking fevers and vocal and motor tics. Her own experience was so different from her son’s, it was hard to believe the same condition could be to blame. “I just thought, ‘It’s really coincidental that I never got well, and now I’m getting worse,’” she says.
She saw a doctor in Cyprus, where her family was living at the time, and then in Saudi Arabia, where her husband was working. Neither visit yielded much. Then, after Robertson’s family moved to Scotland in the summer of 2023, a specialist there diagnosed with Long COVID. She is still sick—and a reinfection late last year set her back—but she has found some relief in treatments prescribed by her doctors, including heart medication and antihistamines.
Robertson’s story highlights the many challenges of detecting, diagnosing, and treating Long COVID. It affects people from all walks of life and produces a vast array of symptoms that can range in severity from mild to life-altering. And because there are so many forms Long COVID can take, it can be difficult for patients and doctors to know what’s going on.
That means many people aren’t getting diagnosed or treated, says Nisreen Alwan, a professor of public health at the U.K.’s University of Southampton who studies Long COVID (and has had the condition herself). Alwan’s research suggests there is “considerable self-doubt” among Long COVID patients, with many people questioning if they should get medical care or have the condition at all. That may be in part because media coverage tends to showcase a specific type of patient—someone who is very sick, potentially to the point of being bed-bound, and battling extreme fatigue and brain fog—so people with milder or more unusual symptoms aren’t sure whether their illness counts as Long COVID, Alwan says.
It’s hard to blame people for being confused. Long COVID is so broadly defined that virtually any unexplained health issue that comes after a case of COVID-19 and lasts at least a couple months could fit the bill. More than 200 symptoms have been linked to Long COVID—everything from insomnia and hallucinations to tremors and gastrointestinal issues—and they often look very different from those of an acute COVID-19 case. Further complicating matters, some people feel better for weeks or months after their initial infection before their health deteriorates.
Research suggests certain symptoms are particularly telltale signs of Long COVID, including fatigue, energy crashes after physical or mental exertion, brain fog, chronic cough, and changes to smell and taste. (These symptoms are also among those the U.S. Centers for Disease Control and Prevention says are most common.) But there’s no universal experience of Long COVID, says Dr. Leora Horwitz, a professor at the NYU Grossman School of Medicine who researches the condition through the federal RECOVER Initiative. “Undoubtedly, there are [patients] who have maybe only one of these symptoms, or maybe a totally different symptom,” Horwitz says.
Symptom severity can vary widely, too. Some people are disabled due to Long COVID, while others live fairly normal lives—at least outwardly. Some people’s symptoms also wax and wane, varying from day to day or going dormant for a while before coming back.
Research suggests about a quarter of the millions of U.S. adults with Long COVID report “significant activity limitations” that affect their ability to work, take care of their families, or carry out other day-to-day tasks. But many people have problems that don’t quite meet that bar, according to a 2023 study that identified four levels of Long COVID: “a few lingering issues,” “significant physical symptoms,” “ongoing mental and cognitive struggles,” and “numerous compounding challenges.” In a group of about 600 Long COVID patients, more than 100 fell into each category, which shows the diversity of Long COVID experiences, says study co-author Keri Vartanian, who leads the Center for Outcomes Research and Education at the multi-state Providence health system.
It’s important for both patients and clinicians to know that Long COVID can take so many different forms, Vartanian says, because recognition is the first step to diagnosis and treatment. Lots of people suffer from many disparate health problems, but it “might not be a multitude of symptoms that somebody is experiencing,” Vartanian says. “It might be one or two things. It might be mental health and only mental health.”
Even if someone is properly diagnosed, of course, there’s no promise that they’ll completely recover—as of now, there’s no cure for Long COVID. Even so, some post-COVID complications, such as damage to a specific organ, can be effectively treated, says Dr. Stanley Martin, an infectious disease doctor who treats Long COVID patients at Geisinger Medical Center in Pennsylvania. Some symptoms that can’t be cured can also be managed to improve overall well-being, he says. (And if someone’s symptoms turn out to be related to something other than Long COVID, that’s worth knowing, too.)
“This isn’t like strep throat, where I’m going to give you a week of penicillin and you’re going to be a new person,” Martin says. “This is going to happen over months and months and months, but we expect and hope to see gradual progress.”
At the very least, receiving a Long COVID diagnosis can provide mental relief. That was the case for Lisa Vargas, a 51-year-old in Washington State who developed Long COVID in 2022. At first, she was so confused and scared by her symptoms—including extreme nausea after eating, stomach pain, excessive mucus production, fatigue, and brain fog—that she hesitated to even tell her family. At times, she wondered if she had dementia.
After being repeatedly dismissed by her primary care doctor, she finally saw a physician who referred her to a Long COVID clinic in Oregon. She’s now gotten some treatments that help, at least temporarily—but just as importantly, Vargas says, she no longer feels isolated by her disease.
“Even when you feel like you’re the most alone because you have the most weird, obscure thing going on,” she says, “I guarantee someone else has it.”
“}]]
The condition’s symptoms and severity can vary widely.
Uncategorized, COVID-19, healthscienceclimate
Health – TIME
The condition’s symptoms and severity can vary widely.
Read moreEnglish News: From COVID-19 to Measles, Florida’s War on Public Health
English News: From COVID-19 to Measles, Florida’s War on Public Health
[[{“value”:”
The culture of public health and medicine rests on open discussions in which different points of view are considered for the betterment of patient care and health. This process depends on psychological safety so individuals feel free and safe to speak and openly disagree. These factors collectively create a just culture, which improves systems and organizations and is being widely implemented in healthcare nationwide.
[time-brightcove not-tgx=”true”]
However, in the face of politicized anti-science and anti-expert sentiment and attacks, we need to ask if just culture is being restricted in public health. Following a series of legislative policy changes in Florida affecting academic institutions, health care, and public health, we see a regression in the open dialog of medical and public health experts about infectious disease control practices related to COVID-19 and now measles.
On January 3, 2024, in marked opposition to the CDC, FDA, and medical and public health experts, State Surgeon General Dr. Joseph Ladapo recommended that everyone avoid COVID-19 mRNA vaccines over concerns that they contain DNA. This notion starkly contrasts ample scientific data showing that these vaccines do not alter a person’s genes, even if they contain minuscule amounts of DNA related to vaccine production. This announcement came on the heels of an earlier announcement on September 13, 2023, recommending that individuals younger than 65 not receive the updated COVID-19 vaccine, even though 25% of COVID-19 deaths have occurred in those younger than 65. Previously, he recommended that young adult men avoid the vaccine because of concerns about myocarditis. However, this risk of myocarditis is very rare, and the risk of myocarditis following COVID-19 is far greater than after vaccination.
Following these announcements, there was broad national criticism of these Florida-only policies. In contrast, the response by the Florida medical and public health community to these controversial recommendations, either in support or opposition, was modest. This tepid response contrasts the first years of the pandemic, when Florida medical organizations, medical schools, and public health experts often commented publicly about the state’s COVID-19 mitigation and vaccination policies.
Currently, there is a measles outbreak in a South Florida elementary school. Dr. Ladapo, not the county health officer, has stated that children at high risk for getting measles can attend school while potentially being contagious, leaving the decision to the parents. Although we are early in this outbreak, we are observing a similar situation where there is considerable national outcry against his recommendation, while the response from the Florida medical community is limited to a few practitioners.
Measles is a very contagious virus, 5 to 10 times more contagious than COVID-19, as it travels long distances and lingers in the air for hours. If an unvaccinated individual is exposed, there is a very high chance that the person will get the virus, which can result in encephalitis, pneumonia, and hearing loss.
Reflecting anti-vaccine and anti-science activity that has become part of the political agenda, rates of measles vaccination among young children have fallen below critical levels in many parts of the US. Not surprisingly, there has been a recent rise in measles cases in the US. The medical community overwhelmingly supports childhood vaccinations but is drowned out by policies that weaken vaccination requirements and misinformation that erodes confidence in vaccines.
Measles outbreaks can be controlled through early post-exposure vaccination measures and quarantining unvaccinated and exposed individuals for 21 days, spanning the incubation period. This recommendation is based on the fact that individuals with measles can be contagious for several days before they show symptoms. Even though more than 90% of the population may be vaccinated against measles in some parts of the U.S., those who are unvaccinated or medically compromised are at high risk if exposed, irrespective of community vaccination rates.
Having a child out of school for three weeks is a long time. Yet, coming out of the pandemic, we have widely available tools to facilitate remote learning, which the school has implemented. When parents do not feel comfortable that an outbreak can be controlled, it is natural for them to keep their children out of school. It was reported that almost 20% of the student body was absent several days after this outbreak, even in this school, which had previously reported high vaccination rates. Was it considered that emphasizing standard measles control policies are being followed, rather than allowing children with potential measles to go to school, could boost attendance?
We need to ask what has happened over the past year to discourage the airing of views contrary to state policies. Is there self-censorship or external censorship? Was there opposition to these recent recommendations by Dr. Ladapo from inside the Florida Department of Health? The answer may lie in reviewing recent legislative and state actions that may give medical experts and those at academic institutions pause in speaking out.
First, a law was passed allowing faculty tenure to be revoked at state universities, meaning faculty with secure positions can now be fired. Florida University faculty members have stated that this policy limits the freedom of experts to speak openly over fears of retribution.
Second, the Medical Freedom bills signed into law in Florida on May 11, 2023, now allow physicians to make public, unsubstantiated, and false claims without consequence. Medicine has regulated itself to keep the public safe. Without these guardrails, inaccurate information can increase without the proper checks of hospital credentialing boards and medical societies. Does this new law make physicians powerless to challenge false and potentially harmful medical information?
Third, the state regulates hospital funding and Medicaid patient care reimbursement rates. University, medical school, and hospital leadership administrators may thus be concerned when faculty members speak publicly and run afoul of political leaders.
Fourth, we see the state dictating what can and cannot be taught at K-12 schools and public universities, something unheard for college and universities in the past. Recently, the Florida Board of Governors banned sociology from the core curriculum of the university system. Considering that the most popular majors at the University of Florida, for example, are psychology and biological sciences, for which sociology is foundational, one needs to ask if the state policy is in the student’s best interest.
Fifth, healthcare providers are now being drawn into culture wars. Medical organizations are also being investigated for health-related issues at the state and national levels.
We now see what happens when policies threaten the perceived ability of medical experts, university experts, medical societies, and public health employees to speak openly. Public discussion about crucial public health state policies fades.
Florida once took its place among the states with the highest COVID-19 vaccination rates for those older than 65 in the US and was among those with the lowest COVID-19 death rates per capita, ranking 29th in the spring of 2021. In contrast, Florida currently has one of the lowest booster COVID-19 vaccination rates in the U.S. and ranks 8th in COVID-19 deaths per capita. Now, Florida has a serious measles outbreak and is not following standard measures of infection control by allowing potentially contagious children to return to school.
Considering the high vaccination rate of 97% at the outbreak site, this outbreak will be contained. But what will happen when measles lands in a school or community with lower vaccination rates and standard public health measures need to be followed?
Do we really want to limit discussions about infectious disease control policies? We have learned the clear advantages of a culture that considers different viewpoints in medicine and public health.
“}]]
A measles outbreak in a Florida school reveals the chilling effect of the state’s turn against public health.
Uncategorized, freelance
Health – TIME
A measles outbreak in a Florida school reveals the chilling effect of the state’s turn against public health.
Read moreEnglish News: Peru Declares Health Emergency in Most Provinces as Dengue Cases Soar
English News: Peru Declares Health Emergency in Most Provinces as Dengue Cases Soar
[[{“value”:”
LIMA, Peru — Peru declared a health emergency in most of its provinces on Monday due to a growing number of dengue cases that are occurring at a time of higher than usual temperatures caused by the El Nino weather pattern.
According to the nation’s health ministry, the number of dengue cases registered during the first seven weeks of this year is twice as high as during the same period in 2023 – with more than 31,000 cases recorded.
[time-brightcove not-tgx=”true”]
“This is a grave problem,” health minister Cesar Vásquez said last week, before the emergency was declared. “And it is getting out of hand.”
The health emergency will enable the nation’s government to transfer funds faster to the affected regions and also transport doctors and nurses. It will cover 20 of the country’s 24 provinces, including regions that surround the capital city of Lima.
A dengue epidemic last year put Peru’s public health system under strain as thousands sought care in emergency rooms.
The disease is spread by Aedys Egypti, a mosquito that reproduces in hot and humid conditions.
Although most dengue cases present light symptoms, the disease can cause severe headaches, fevers and muscle pains.
Last year, a dengue epidemic in Peru killed 18 people, while in the first two months of this year 32 Peruvians have died from the virus.
In December, the World Health Organization said that Peru’s 2023 dengue epidemic was linked to rains and hot temperatures that helped mosquito populations to grow, especially in the north of the country.
“}]]
The declaration applies to most of the country’s provinces at a time of higher than usual temperatures caused by El Nino.
Uncategorized, wire
Health – TIME
The declaration applies to most of the country’s provinces at a time of higher than usual temperatures caused by El Nino.
Read moreEnglish News: Here’s What Americans Think of Weight Loss Drugs
English News: Here’s What Americans Think of Weight Loss Drugs
[[{“value”:”
Not every major medical innovation breaks through to the general public. But the buzzy weight loss drugs for people with obesity or Type 2 diabetes certainly have.
About 75% of Americans have heard of Ozempic, Wegovy and other brands of anti-obesity drugs, according to the results of a new Pew Research Center survey. (Wegovy and Zepbound are specifically approved to treat obesity, while Ozempic and Mounjaro are approved to treat people with Type 2 diabetes and can help them lose weight.)
[time-brightcove not-tgx=”true”]
The survey included more than 10,000 people of different ages, genders, races, ethnicities, education levels and political affiliations who were randomly recruited to answer online questions about obesity and the new class of anti-obesity medications.
Among those familiar with the drugs, 53% said they were good weight-loss options for people with obesity, while 28% were unsure—and 62% said they were not good options for people without a weight-related health condition. That last stat reflects the controversial, widely publicized trend of people without these conditions taking the drugs as a quick way to lose weight.
Read More: More Weight Loss Drugs Are Coming, and They Could Be Even More Effective
When asked what impact the drugs would have on reducing obesity in America, 35% thought they would do “not much” or “nothing at all,” and only 16% thought the medications would do “a great deal” or “quite a bit.” “Those expectations are fairly modest and could change, since these medications are still fairly new,” says Alec Tyson, associate director of science and society research at the Pew Research Center.
But the survey shows that “the public has a nuanced take on the factors that influence weight,” Tyson says. Most survey respondents (57%) said diet affects a person’s weight “a great deal,” with exercise following as the next most important factor at 43%. Many (36%) said that stress and anxiety affected weight “a great deal,” and 22% said genetics did. Past research has found that all of these factors matter. An even larger percentage, 65%, acknowledged that willpower is not enough to lose weight and maintain a healthy weight.
That’s where anti-obesity medications could play a role, says Tyson. “The survey suggests there is a fair amount of openness among Americans for this new group of drugs designed to address food cravings to address obesity and overweight in this country.”
“}]]
A new Pew Research survey polled Americans on the latest class of drugs.
Uncategorized, healthscienceclimate
Health – TIME
A new Pew Research survey polled Americans on the latest class of drugs.
Read moreEnglish News: An Asthma Drug Can Drastically Reduce Food Allergies
English News: An Asthma Drug Can Drastically Reduce Food Allergies
[[{“value”:”
About 20 million people in the U.S.—including four million children—have food allergies. Now, there’s a new way to reduce their risk of severe allergic reactions. A study published in the New England Journal of Medicine reports that the drug omalizumab, or Xolair, allows people with food allergies to tolerate higher doses of allergenic foods before developing a reaction after an accidental exposure. It also leads to milder reactions if they are exposed.
[time-brightcove not-tgx=”true”]
The drug was originally approved more than two decades ago to treat allergic asthma. But because of this new study and other data, the U.S. Food and Drug Administration expanded the approval of Xolair on Feb. 16 to include treatment of food allergies in anyone one year or older. It’s now the first drug approved to treat allergies to multiple foods.
Anabelle Terry, a 12-year old with severe peanut and tree nut allergies, experienced that benefit firsthand as a participant in the trial. While participating in the study, she ate half a cupcake while with friends that she thought was nut-free but had made been made with cashew flour. Within about an hour, her stomach and throat started to hurt and her lips tingled, so she thought she was having an allergic reaction and went home. Her mom gave her an antihistamine, which was enough to quell her symptoms. Before Xolair, if she ate even a tiny amount of peanuts or tree nuts, she would generally need a shot of epinephrine, which is an emergency treatment for an allergic reaction, and a visit to the doctor. “I did notice a difference—I didn’t react as badly as I thought I would have,” Terry says. “I only had half, but it was a big cupcake, and it was amazing to see that even though I accidentally ate some, I was okay.”
Xolair does not cure food allergies, so people must continue to avoid allergy-causing foods by reading labels and asking how food is prepared. But people now “have another layer of protection in case of accidental exposure,” says Dr. Sharon Chinthraja, associate professor of medicine at Stanford University School of Medicine and co-lead of the study.
How Xolair works to fight allergic reactions
The drug works by mopping up something called immunoglobulin E (IgE) cells, which activate the immune cells responsible for inflammation and allergic reactions. “I think of the drug as a sponge that takes allergic antibodies out of circulation,” says Chinthraja. It was this mechanism that led to Xoalir’s original approval in 2003 for allergic asthma, since IgE cells play a role in that condition as well. “There were suggestions that the drug should work in food allergy too, but no study until this one demonstrated that to the level required by the FDA to add it to the label, says Dr. Robert Wood, director of pediatric allergy, immunology, and rheumatology at Johns Hopkins Children’s Center and the principal investigator of the study.” In fact, because of the way the drug blocks IgE, it “may be more applicable to food allergies because asthma has a lot of different triggers, but food allergies are pretty much an IgE-driven reaction.”
What the new study shows
The study included 177 children from ages 1 to 17 at 10 different sites in the U.S. The participants were randomly assigned to receive Xolair as an injection either every two weeks or every four weeks, depending on their body weight and levels of IgE (a proxy for how severe their food allergies are), or a placebo. All of the participants were allergic to peanuts and at least two other foods such as tree nuts (cashews, walnuts, and hazelnuts), milk, eggs, or wheat. After about four months of receiving the injections, the kids were given high levels of peanut or other food allergens—much higher than doses they might encounter by accidentally taking a bite of food containing them. Of those who took Xolair, 67% were able to tolerate the higher dose of peanut without a severe allergic reaction, compared to 7% of those getting placebo. The breakdown was similar for the other allergens.
“Over half [of the participants] could eat a lot of the foods they were allergic to,” says Dr. Robert Wood, director of pediatric allergy, immunology, and rheumatology at Johns Hopkins Children’s Center and the principal investigator of the study. “More than 50% could eat the equivalent of 16 peanuts with no reaction.” Among the remaining half, about 15% experienced allergic reactions even at small doses of exposure, but all of the reactions were milder among the Xolair group than the placebo group. It’s not clear how long the drug blocks IgE activity, but doctors anticipate that people will have to continue getting the shots to lower their risk of severe reactions.
How to use Xolair for food allergies
For Anabelle, the drug provides a sense of security. “I’ll be able to try new things and do some things that I wasn’t able to before,” she says. “I love traveling even more now because I don’t always have to worried about whether a new food is safe. I’m still cautious, but more free to experience things.”
Xolair isn’t an emergency treatment. It’s designed to be a maintenance therapy that keeps the immune system in check for as long as people take the medication, so that if someone is accidentally exposed to an allergy-causing food, their reaction will be dampened and not life-threatening. The first few doses might be given at the doctor’s office to make sure people don’t have adverse reactions to the shot, but parents give subsequent doses to children at home. Adults can also give the shots to themselves.
To work, a person has to keep taking the shots. That can get expensive: A spokesperson for Genentech, which makes the drug, says the injections for food allergies will cost the same as those for asthma, which amounts to $2,900 for children and $5,000 for adults each month. It’s not clear yet whether insurers will cover Xolair for treating food allergies, but many do cover the drug for asthma. For the uninsured, Genentech offers a patient assistance program.
Anabelle’s parents are still discussing with their allergist how Xolair might fit into her life. Anabelle completed the trial in 2022 and has not taken the drug for two years. “I would be willing to go back on it,” she says. “Maybe with more treatment, it could become even less severe and make me less stressed about food.”
“}]]
The drug could become an important safety net for millions of people with food allergies.
Uncategorized, healthscienceclimate
Health – TIME
The drug could become an important safety net for millions of people with food allergies.
Read moreEnglish News: How Technology Can Help Us Remember Better
English News: How Technology Can Help Us Remember Better
[[{“value”:”
In the digital age, we have the technology to document our lives in extraordinary detail via photographs, voice recordings, and social media posts. In theory, this ability to effortlessly capture the important moments of our lives should enrich our ability to remember those moments. But in practice, people often tell me they experience the opposite.
I study the neuroscience of memory and one question I hear again and again is whether technology is making us “dumber”—or, more precisely, whether it’s hurting our ability to remember. For some, the question is motivated by worry about the amount of time their children spend on screens or mobile devices. For others, it reflects concerns about their own memory problems.
[time-brightcove not-tgx=”true”]
A common fear is that there might be a “use it or lose it” principle at play—that an increasing dependence on our devices for reminders will lead us to lose our own capabilities to remember. This might be true for certain skills. If, for instance, you always rely on navigation apps in new or unfamiliar neighborhoods, you might not attend to features in the environment to create a mental map that would allow you to learn to navigate on your own. However, there is no reason to think that relying on technology to store important information will somehow lead your brain to wither in ways that are bad for memory. In fact, I’m all for outsourcing mundane memory tasks, like memorizing phone numbers, passwords, email addresses, and appointments. I don’t have a photographic memory—but my phone does.
So, if technology can help us “free up space” for the things we want to remember when we need to remember them, why do so many of us feel like its presence in our lives is leading us to form blurry, fragmented, and impoverished memories?
The short answer: technology isn’t the problem—it’s how we interact with it.
To form lasting memories, we need to focus on what is distinct about the present moment, those immersive sensory details we can call back up to reconstruct an experience when we remember. As we go about our daily lives, we usually do a pretty good job of focusing on what’s relevant, and for that, we can thank a part of the brain called the prefrontal cortex. The prefrontal cortex helps us focus attention on and meaningfully process what we need to learn, to search for memories that are “in there somewhere,” and to keep our recollections accurate when we manage to remember the right thing.
But, in a world where our conversations, activities, and meetings are routinely interrupted by text messages, emails, and phone calls, these abilities get swamped—and we often compound the problem by splitting our attention between multiple goals. Multitasking can make us feel that we’re being more efficient. Many of us even pride ourselves on our ability to switch from one task to another, but it comes at a cost.
Read More: Why Multitasking Is Bad for You
Each time we are routinely distracted or intentionally toggle between different media streams (such as reading a text message while maintaining a conversation), prefrontal resources are sucked up to regain our focus. The result is that we remain one step behind, and after all is done, we are only left with blurry, fragmented memories.
Outside of the workplace, we often use technology to document our lives. The proliferation of “Instagram walls” and the throngs of people at concerts recording the action with their smartphones illustrate how technology has changed our lives. The ubiquity of smartphone cameras enables us to easily document our experiences, yet for most of us this hasn’t translated into a more expansive memory for the personal past. Again, the problem isn’t necessarily with the technology, but rather that we are filtering our experiences through the lens of a camera.
Taking photos does not necessarily have a good or bad effect on memory. The critical factors involve how you direct your attention and whether you meaningfully engage with the subject matter. Our brains are designed to do more with less, by engaging meaningfully with a little bit of high-quality information rather than amassing a massive catalog of information. When we focus on “documenting” over “experiencing,” we don’t pay attention to what is distinctive in the moment, the sights, sounds, smells, and feelings that make an experience unique—and memorable. Without those immersive details, something that was so vivid when we experienced it (a family vacation or child’s violin recital) can wind up feeling as distant to us as a story we read in a book. By trying to record every moment, we don’t focus on any one facet of the experience in enough detail to form distinctive memories that we will retain.
The negative potential of technology is exacerbated by a culture of sharing experiences on social media platforms. Social media engagement can have a negative effect on memory, partly because it involves multitasking (e.g., switching between recording the moment and engagement with social media platforms) and increases the potential for distraction.
Social media itself isn’t bad for memory, per se. Like most forms of technology, it’s a tool that when used properly can even enhance our memory of an event, but the images we post are often accompanied by captions with brief descriptions, rather than a thorough reflection on the event. Some platforms like Snapchat and Instagram stories, feature photo posts that disappear within 24 hours—an apt metaphor for the way in which mindless documentation can leave us bereft of lasting memories for our experiences.
Read More: How to Make Your Mind Happy, According to Neuroscience
Technology can enhance memory if it is used consistently with principles that help us remember. Thoughtfully taking pictures or videos at opportune moments can orient us to what is interesting and distinctive around us. My daughter, for instance, likes to selectively photograph plants and flowers that catch her eye on our nature walks, which allows her to pause and fully take in those aspects of the scenery as we are experiencing them in the moment.
After you take those pictures and videos, organize them in a way that will allow you to find them later (as we used to in the old days with photo albums) and make sure to revisit them later on. In the following weeks, revisit those photos and use them as cues to mentally re-experience those events, bringing back as many details as possible. By using the photos almost like a “test” of your memory, and spacing out those tests, you can enhance your ability to retain memories of the entire event, not only what is in the photo. Journaling can be another way to enhance memory because it allows us to test our memory for an event and also integrate it in a meaningful way, so that we can shape our narrative of the experience.
As with memory itself, a key principle for technology is that “less is more.” All the life-logging in the world will not enable us to remember all our experiences, nor is that a desirable goal in the first place. Our memories for events are selective, but they also can have a great deal of detail, meaning, and emotion. By mindfully using technology in ways that allow us to access those aspects of our past experiences, we can hold on to what matters.
“}]]
Mindfully using technology to access past experiences can help us hold on to what matters, writes Charan Ranganath.
Uncategorized, freelance
Health – TIME
Mindfully using technology to access past experiences can help us hold on to what matters, writes Charan Ranganath.
Read more