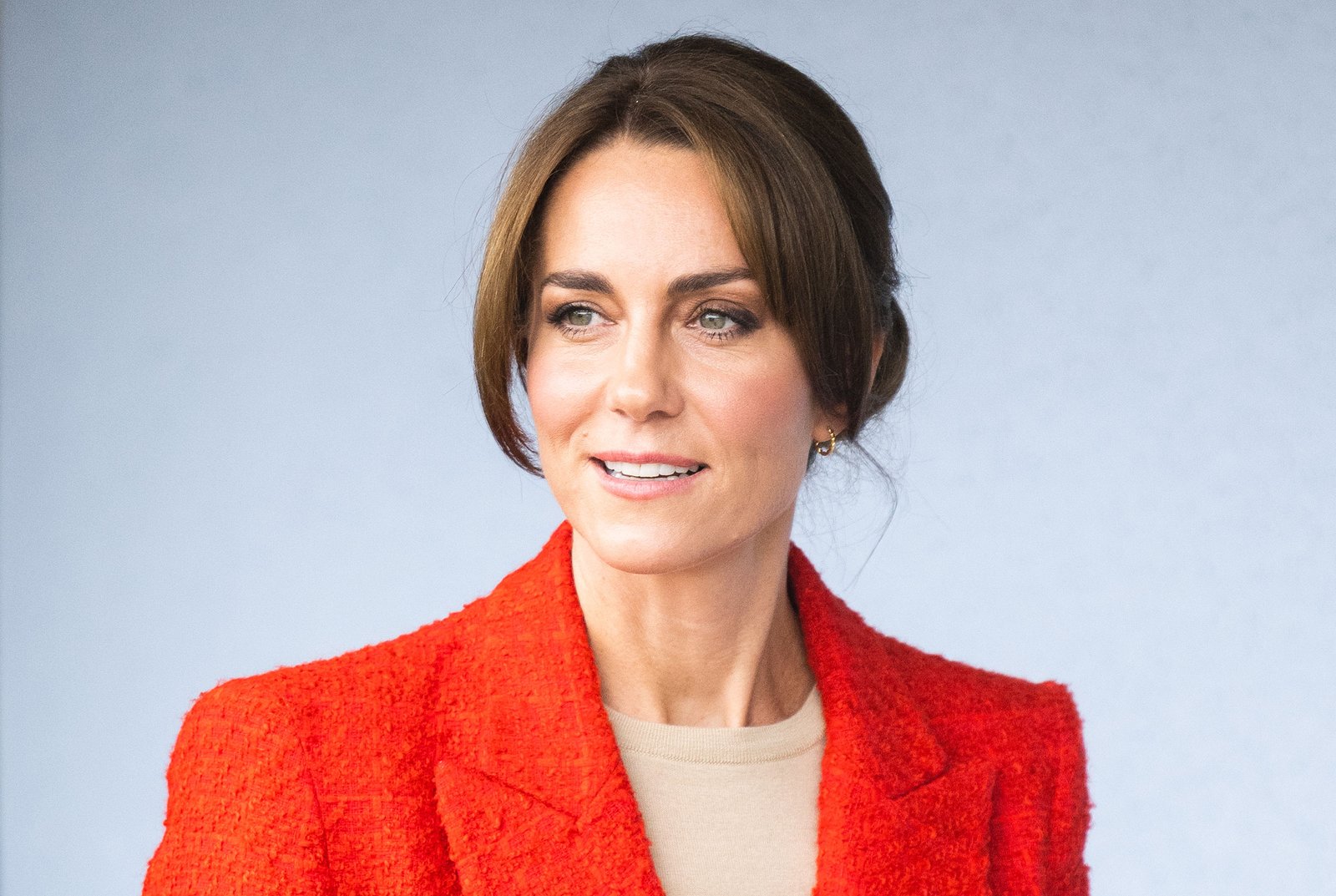
English News: Kate Middleton Had to Tell Her Kids About Her Cancer Diagnosis. These Parents Know What That’s Like
English News: Kate Middleton Had to Tell Her Kids About Her Cancer Diagnosis. These Parents Know What That’s Like
[[{“value”:”
After weeks of fevered speculation, Catherine, Princess of Wales, revealed on Mar. 22 that she was absent from the public eye not because she was having marital problems or growing out a bad haircut, but because she was being treated for cancer. She and her husband had, she said, “taken time to explain everything to George, Charlotte and Louis in a way that is appropriate for them, and to reassure them that I am going to be OK.” Even before her announcement, however, many cancer survivors who were also parents had already guessed at the truth. The silence and delay tactics looked familiar, because they had done the same thing when they got their own diagnosis.
[time-brightcove not-tgx=”true”]
“When you hear cancer, you just think, ‘Oh, my goodness, I’m going to die,’” says Shambi Broome of Columbia, S.C., who was diagnosed at age 46 with colon cancer after a routine scan in 2022. “And then the next thought is, ‘Wow, how do I tell my kids?’” Broome, who didn’t know the full extent of her cancer until after she had an operation, waited until she was told she’d need chemotherapy before mentioning the C-word to her children, who were 13 and 18 at the time. Instead she told them she was having a part of her colon removed. “I didn’t want to tell them anything until I could give them a full story,” she says. “I didn’t know what I would be preparing them for and I didn’t want to scare them.”
Read More: Kate Middleton Is Receiving Preventative Chemotherapy. Here’s What That Is
That was also the case for Fiona Williams, some of whose children, at 17, 8, and 6, were close in age to the Windsor offspring when she was diagnosed in 2021. She mentioned nothing to them about her endometrial cancer until after her hysterectomy when she was told doctors had missed some and she’d need a further operation plus chemotherapy. “At that point, I thought that I’m going to have to tell my children now, because they’re going to see me going through chemotherapy,” says Williams, now 48. She tried to put as positive a spin on the news as she could, as they had already lost two relatives to cancer. “Of course the kids just start straightaway start crying, ‘Oh, you’re going to die, you’re going to die,’” she says.
Williams, who is Scottish, says she feels particular sympathy for Middleton, because the announcement reminded her of her own medical procedure. “As soon as they said she was having ‘abdominal surgery,’” I said to my husband, ‘I bet you it’s some sort of cancer,’” she says. She understood the need for obfuscating the real reason for Middleton’s reclusiveness. “I knew that’s why they were keeping it quiet. She didn’t have to publicly tell people. I think it’s just such a shame that she’s been forced into doing that.”
Cathal Morrow handled it somewhat differently when he was diagnosed in 2018. As a single dad looking after his children full-time, the Londoner felt he needed to tell his children, then 13 and 11, as quickly as possible. So he sat them down the evening after he was told the weird lump in his groin was T-cell lymphoma. “I said, ‘Look, this is the situation. I have cancer. It’s a great hospital. We don’t know how it will turn out,’” says Morrow, now 58.
Read More: Why Are So Many Young People Getting Cancer? It’s Complicated
While his approach may sound brutal, he said it was advised by a brochure from a cancer charity that he picked up at the oncologist’s office to be honest with his children. And he emphasized the theme of security. “It was like, ‘Whatever happens, you’re going to be safe. Whatever happens, you’re going to be secure.’ I was positive without being dishonest,” Morrow says. “And the kids were amazing. I think there’s a certain amount of denial that kids have.”
Because of the ages of Kate and William’s children—George is 10, Charlotte is 8, and Louis is 5—the royal family would probably have had to tread more carefully than Morrow, a PR exec who once went a year without lying as an idea for a book. (He decided against writing it.) “The thing is, if you lie to your kids and say everything’s gonna be great when you don’t know, in the short term that definitely helps,” he says. “But then, if you end up slowly dying, then actually I think you’ll do your kids more damage.”
Parents noted that their family anchor during their cancer treatment was normality, which may be a little harder for the Duke and Duchess of Cambridge to manage than most people. “My goal was that I didn’t want it to interrupt my kids’ routine,” says Broome, whose treatment became complicated when a case of COVID-19 and a dose of chemo coincided and her health spiraled downward. “I would be physically present even if I wasn’t feeling great or wasn’t always there, but you try to do your best.”
Read More: Kate Middleton and Prince William Break Silence After Cancer Diagnosis Reveal
That’s not to say it’s easy. Many parents struggled with maintaining a carefree attitude while being afraid they were in their last days. Morrow recalls that one of his sons declined to watch one of the Matrix movies with him and his other son the Saturday night after he got his diagnosis. “I went to the kitchen, and I burst into tears,” he says. “And I realized that I wanted to watch The Matrix with my boys before I died.” The revelation helped steer him away from letting his fear affect his interactions with his children. “The hardest thing with the kids was, if I was going to die, not to treat everything like it was my last moment,” he says.
But parents also cautioned that you can’t always tell how the news of the illness is affecting a child. Fran Hawthorne, a writer in New York City, thought her 10-year-old son was handling it really well after she told him she had breast cancer in 2005. He had lots going on in his life and was transitioning from elementary school to middle school. But halfway through summer camp, when she and her husband brought him home for a scheduled weekend visit, he suddenly announced he didn’t want to leave. She was stunned because he’d loved summer camp and had begged to go for an extra session the year before. Eventually, though, she put two and two together. “When I showed up, it triggered something subconscious in him,” she says. “He was like, ‘Oh my God, if I’m away from mom, she could die while I’m away!’” she says. She let him stay home.
Broome, whose treatment finished only six months ago, says she has no regrets about how she handled her illness, but still feels what she calls “cancer guilt” on top of the usual mom guilt. “I thought they were OK,” she says of her kids, with a catch in her throat. “And then my youngest said, ‘I thought you were going to die,’ and I felt like I didn’t protect them enough.” She’s not sure there is a right answer for how much to tell children, especially when they’re younger. “If you think you’re protecting them, maybe it’s not enough information, so they’re coming up with their own scenarios,” she says. But telling them too much can be equally overwhelming. “No matter how much you think you’re protecting your kids,” says Broome, “when you have cancer, you’re really not.”
“}]]
Kate Middleton had to share her diagnosis with her children. These parents have been there.
Uncategorized, Cancer
Health – TIME
Kate Middleton had to share her diagnosis with her children. These parents have been there.
Read moreEnglish News: Why So Many Dogs Have Allergies Now
English News: Why So Many Dogs Have Allergies Now
[[{“value”:”
Every day, itchy dogs shuffle into Elizabeth Falk’s veterinary office. Some can’t stop chewing their feet or scratching their bellies. Others have red, smelly ears, or rashes on their skin. All are intensely uncomfortable because of environmental allergies. “They’re sitting in the waiting room, and everyone else is backing away out of fear that it’s contagious,” she says. “It’s super busy helping as many as we can.” Until recently, Falk was a veterinary dermatologist at Cornell University Veterinary Specialists, where she saw about 15 allergic pets a day and was booked up to six months out. Demand is so high that in April, she’ll open her own pet dermatology practice.
[time-brightcove not-tgx=”true”]
More and more dogs are suffering from atopic dermatitis, otherwise known as environmental allergies: According to a 2018 report from Banner Pet Hospital—the latest U.S. numbers on the subject—there’s been a 30% increase in cases over the past 10 years. In 2021, a teaching hospital in Brazil reported that 25% of dogs they examined suffered from allergies. Though dog allergies aren’t consistently tracked, anecdotally, they’re soaring. “Allergic skin disease is probably the top thing we see,” says Erin Tate, vice president of clinical development at CityVet in Dallas. “I’ve been doing this for 25 years and have definitely seen a dramatic increase in recent years.” Dogs with environmental allergies tend to be “miserable,” she adds, sometimes scratching so aggressively that their hair falls out. Spring is a particularly trying time. “I tell people that if your allergies are flaring up, your dog’s allergies are flaring up, too,” Tate says.
But what’s driving the increase in itchiness? And what helps relieve allergic dogs’ agony?
Some dogs are allergy magnets
There’s a strong genetic component to atopic dermatitis, Falk says. Certain breeds are prone to them, including German Shepherds, Labrador Retrievers, French Bulldogs, English Bulldogs, West Highland Terriers, Shih Tzus, pitbulls, pugs, and Boxers. Allergies look different in different breeds. German Shepherds, for example, tend to get crusts around their lips, Falk points out, while labs develop bumps between their toes.
Read More: Dog Owners Live Longer, Healthier Lives
Environmental allergies typically first appear when a dog is 6 months to 3 years old, says Matthew McCarthy, founder of Juniper Valley Animal Hospital in Queens, though there are outliers. Allergies are the result of skin barrier dysfunction, or a defective outer layer broken down by inflammation. “The old-school way we used to think about this was, these guys are inhaling [allergens], and they’re getting into their bloodstream, and they’re reacting, and that’s what’s causing the histamine to be released,” McCarthy says. “Now, we know that’s probably not the case.” Instead, airborne allergens—like pollen from grass or trees—likely get absorbed through the dogs’ skin. That leads to symptoms such as excessive itchiness, which might prompt dogs to constantly lick or chew their feet or rub their faces. In some cases, atopic dermatitis manifests as frequent skin and ear infections rather than itchiness; an especially unlucky group of dogs experience all of the above.
Climate change plays a role
The main reason why an increasing number of dogs suffer from allergies has to do with the warming planet. “Allergy season has been extended because of climate change and the dramatic change in temperatures,” Tate says. During the winter where she lives in Texas, there might be a couple cold days in the 30s or 40s, immediately followed by a jump to the 70s or 80s. “Every time we get that warm spell in between the cold, stuff starts to bloom again,” she says. “Nothing ever gets a chance to die.”
Read More: Why Allergy Seasons Are Getting Worse
Research suggests that warmer weather and increased carbon dioxide concentrations extend the growing season for mold spores and plants like ragweed, while also worsening air pollution. In North America, pollen seasons now start 20 days earlier and are 10 days longer than they were in 1990. Plus, there’s an average of 21% more pollen during each allergy season. Cue the frantic calls to your pup’s vet. “Climate change is affecting humans and dogs,” Tate says.
Dogs used to get dirtier than they do now
Early exposure to microorganisms—through things like dirt, germs, and even dogs—can help protect infants from developing allergies. The same is true of dogs, says Matthew Levinson, a veterinary dermatologist who owns Pet Derm in Chicago. Research suggests that dogs who live in a rural environment, regularly go for walks outside, and have contact with farm animals are less likely to have environmental allergies, while atopic dermatitis is more prevalent in urban environments, where dogs tend to spend a greater amount of time inside.
“We’re more clean and hygienic—dogs aren’t spending as much time outside anymore,” Levinson says. “It’s not like back in the day, where you’d have a dog house in the backyard, and the dog spent most of the day in the yard.”
Meanwhile, dogs who live in a household with other dogs also appear to benefit from a protective effect. But that doesn’t necessarily mean you need to adopt another dog—or try to expose your pet to more germs. It’s difficult to tease apart all the genetic and environmental factors that contribute to allergies, Levinson says. There’s simply “too much variation between the individual dogs, and so much that’s subjective,” he says, making wholesale recommendations tricky.
A silver lining: better treatment options than ever
On any given day, Levinson treats 14 to 17 allergic dogs. He says he feels so guilty knowing how many more are suffering that he often double-books appointments. When an itchy dog arrives in his office, he first takes a detailed history: What areas of the body are itchy, and what times of the year do they flare up? He’ll do a physical exam, looking for redness in their paws and groin, and might suggest an elimination diet to rule out food allergies. Once he’s certain the dog has environmental allergies, he’ll usually advise allergy testing. That means he injects dozens of small amounts of allergens under the dog’s skin, and if the pup is allergic, a hive will form at the site, pointing to the culprit.
Managing allergies is a “marathon, not a sprint,” Levinson stresses, and most dogs require lifelong treatment. There’s no cure, but treatment options are far better now than they were even a decade ago. The majority of dogs respond well to immunotherapy: customized injections, just like the allergy shots humans receive, that train the immune system to become desensitized to certain allergens. It could, however, take more than a year to see results.
Read More: Suffering from Seasonal Allergies? Here’s What Experts Say Works Best
There are other options. In 2013, an oral medication called Apoquel was approved to control itchiness and inflammation in allergic dogs. “It was like a miracle,” Falk says. “We had been waiting for it for so long.” It’s safe and well-tolerated, she adds, and is a “reasonable long-term medication” for itchy dogs who get skin infections.
A few years later, in 2016, another treatment option came on the scene: Cytopoint, a targeted therapy that’s administered via injection every four to eight weeks. It’s a monoclonal antibody to an itch signal called interleukin (IL)-31, Falk explains. “It binds to that itch signal,” she says. “It doesn’t affect the rest of the immune system in any way, which makes it very safe.” The downside, she adds, is that it’s only intended to control itchiness—so allergic dogs prone to infections caused by inflammation will still get them. That’s why it’s important to align medication choices with how a dog manifests allergies: Itchy dogs who never get infections usually do best on Cytopoint, while Falk often prescribes Apoquel for those who do develop infections, since it’s a good anti-inflammatory choice.
However, doggy dermatology doesn’t come cheap, and pet insurance typically only covers treatment if dogs are insured before they become symptomatic. Allergy testing can cost upwards of $1,000 out of pocket, Apoquel is about $90 for 30 tablets, and a Cytopoint injection can range from $50 to $200, depending on the dog’s size.
Is there any way to prevent allergies?
Having an allergic dog typically boils down to bad luck. If a dog is born predisposed to itch, he’s going to itch. But if you’re considering buying a puppy from a breeder, it can be helpful to ask them if there are any allergic dogs in a potential pet’s pedigree, Falk advises. Research suggests that when two dogs with atopic dermatitis are bred, 65% of their offspring will have environmental allergies; if just one parent has the condition, that drops to 21% to 57%; and if neither parent has allergies, 11% will go on to develop problems.
If your dog has allergies (and even if they don’t), make it a point to bathe him regularly—about once a month—to remove potential allergens from the skin, Tate advises. She thinks of dogs as “little dust mops” who pick up a lot when they’re gallivanting around outside. Some people like to wipe their pets down with unscented baby wipes to get the pollen off, she adds.
And, most importantly, if your dog is suddenly scratching a lot more than usual, take him to the vet. Depending on the severity of the situation, your vet might refer you to a specialist, but many cases can be handled by your regular vet. “The earlier you get started with immunotherapy, the better the success rate,” Levinson says. “When the dog is younger, you can mold the immune system a lot easier, versus if you have a dog who’s had allergic symptoms for several years.” The sooner you get on top of your dog’s health, he stresses, the happier you’ll both be.
“}]]
Climate change plays a role.
Uncategorized, healthscienceclimate
Health – TIME
Climate change plays a role.
Read moreEnglish News: How Hypertrophic Cardiomyopathy Progresses in Adults
English News: How Hypertrophic Cardiomyopathy Progresses in Adults
[[{“value”:”
Hypertrophic cardiomyopathy is the most common form of genetic heart disease worldwide. Researchers have estimated that up to 1 in 200 people have the condition, which is characterized by an abnormal thickening of the walls of the heart. This thickening can make it difficult for the heart to pump blood.
Hypertrophic cardiomyopathy can be a deadly disease, and there was a time when it was largely untreatable. But the last 20 years have witnessed a sea change in the condition’s management—a change that has led to an estimated 10-fold decrease in deaths.
[time-brightcove not-tgx=”true”]
“Hypertrophic cardiomyopathy has this reputation that it’s difficult to live with, and that the outlook is grim,” says Dr. Barry Maron, a cardiologist and hypertrophic cardiomyopathy specialist at Beth Israel Lahey Health in Burlington, Mass. “That used to be true, but there have been huge advances in clinical care and clinical research, and hypertrophic cardiomyopathy is now characterized very differently.”
“The reality,” he adds, “is that very few people die of the disease, and fully half of patients belong in a group we consider benign and stable.”
Here, Maron and other experts describe what it’s like to live with hypertrophic cardiomyopathy. They explain the different stages or forms of the disease, how and why it progresses, and how treatment may evolve over time. They also talk about the outlook for people who are diagnosed with the condition.
An unpredictable disease
Some medical conditions—certain forms of cancer, for example—are characterized by different stages. Those stages help determine treatment, and they also reflect a patient’s prognosis.
Experts say hypertrophic cardiomyopathy is different; it doesn’t play by such tidy rules. “It’s an incredibly heterogeneous disease, and the more we learn about it, the more complex it gets,” says Dr. Christopher Kramer, distinguished professor and chief of cardiovascular medicine at the University of Virginia School of Medicine. The condition can affect the physical properties of the heart in different ways, he says, and trying to anticipate how it will behave over time is difficult. “To say to a patient, ‘You’re going to do this, and this is your likely outcome’—that’s fraught,” he adds.
Maron agrees that “there is no average” when it comes to hypertrophic cardiomyopathy. However, he says that the disease can be broken down into four general pathways. “The first pathway is the benign and stable course, and thankfully this is the most common of the four,” he says. These are patients whose disease tends to be caught incidentally sometime in midlife; for example, they undergo some type of medical imaging and their doctor notices an irregularity in their heart function—a heart murmur, for example. This leads to follow-up testing that reveals hypertrophic cardiomyopathy. In these cases, a person’s myopathy may not be obstructive, meaning it’s not limiting blood flow, and it may require little more than follow-up monitoring to ensure it’s not getting worse.
“The second pathway involves heart failure due to some kind of obstruction,” Maron says. In these obstructive cases, a person’s cardiomyopathy restricts the flow of blood out of the heart. These patients often have symptoms such as chest pain or shortness of breath. Symptoms can range from severe to very mild—so mild that a person may live with them for years without thinking much of them. “Patients will say they have no symptoms, but once you start asking questions, you find they’ve never been able to keep up with friends during exercise, or they’re often short of breath,” says Dr. Milind Desai, a cardiologist and hypertrophic cardiomyopathy specialist at the Cleveland Clinic. “A lot of people don’t realize how they’ve adapted their lifestyles to the condition over the years.”
Fortunately, this obstruction-related heart failure is often reversible with the help of either medication or some type of procedure, such as surgery to remove part of the thickened heart muscle. In rare and severe cases, a person’s myopathy may not respond to these treatments; or they may respond well initially, but then the condition eventually grows worse. “A small subset of patients develop advanced hypertrophic cardiomyopathy where the muscle of the heart is thick and stiff and non-complaint, and the only option might be a heart transplant,” Desai says. “But that, mercifully, is only the case in 3% to 5% of patients.”
The third pathway involves people whose hypertrophic cardiomyopathy leads to atrial fibrillation—a condition where the rhythms of the upper and lower chambers of the heart are misaligned. Atrial fibrillation can lead to a stroke if left untreated, and many of these patients will require anticoagulant drugs (such as blood thinners), and perhaps medication or surgery.
“The fourth pathway is someone who is at risk for sudden cardiac death,” Maron says. While identifying these cases still involves some educated guesswork, he says the latest diagnostic tools are very good at identifying at-risk patients. Treatment typically involves implanting a small defibrillator, or ICD, to correct irregular heart rhythms. “Implantable defibrillators have saved countless lives,” he adds.
While these four pathways can help sort people with hypertrophic cardiomyopathy into four rough groups, experts reiterate that the course of the disease is hard to anticipate. However, with proper care, they also say that most people diagnosed with hypertrophic cardiomyopathy will not die of the disease. “At this point, most well-managed patients can expect to live a normal lifespan,” Desai says.
Read More: What to Know About Hypertrophic Cardiomyopathy in Kids
How and why the condition progresses
Here again, experts stress the unpredictability of the disease. “Progression of hypertrophic cardiomyopathy is highly variable,” Kramer says. “It may progress and it may not, and we’re doing studies to understand who is most likely to progress and why.”
People with genetic forms of the condition—meaning those who have inherited one or more of the genetic mutations associated with hypertrophic cardiomyopathy—may have more severe and aggressive disease that often manifests earlier in life. But this isn’t always the case. “There is a portion of patients who have a genetic mutation but never develop the overt disease, and we’d never know they had it if we didn’t look for it,” says Desai. However, among patients with obstructive forms of hypertrophic cardiomyopathy—either with or without symptoms—experts say the condition is likely to get worse if left untreated. The muscle thickening will advance, symptoms will develop or become more severe, and the risk of a person developing atrial fibrillation or other life-threatening complications will increase, he says.
While predicting the course of the disease can be difficult, experts say that people who are symptomatic and diagnosed with the condition at a young age tend to face more challenges than people who are older at the time of diagnosis. “If you’re diagnosed at age 50 or 60, your prognosis is usually good—probably similar to age-matched controls,” Kramer says. “But if you have a family history of the disease and you’re diagnosed at 25, that’s less optimal.”
Other health issues can also advance the disease. Experts say obesity, high blood pressure, and diabetes can make underlying hypertrophic cardiomyopathy worse. “It’s important to stay on the ball with your health,” Desai says.
How treatment may evolve
At the time of diagnosis, most people with hypertrophic cardiomyopathy will have no symptoms and no evidence of an obstruction. Apart from follow-up monitoring, most won’t require treatment.
If the disease progresses—meaning, an obstruction or other threat to the heart arises—treatment may involve an implantable defibrillator, or medications intended to manage symptoms or reduce the risks of complications. For example, the latest anticoagulant drugs have “come close to obliterating” the risk of stroke in people who develop atrial fibrillation as a result of hypertrophic cardiomyopathy, Maron says. Meanwhile, a newer drug called mavacamten can help reduce symptoms, and possibly even reverse some heart-muscle thickening, in people with obstructive forms of the disease. Experts say this drug has helped improve quality of life for many patients, but it’s not a cure-all. “Mavacamten has made a beneficial contribution, but so far there’s nothing about this class of drug that will have a direct effect on mortality,” Maron says.
If a person responds well to the drug, they must stay on it indefinitely and undergo quarterly monitoring to ensure the heart’s functioning is stable. If their heart’s condition worsens or symptoms persist, experts say the next step in treatment is likely to be some kind of procedure. For patients who are younger or those experiencing severe obstruction, doctors may recommend a septal myectomy—an open-heart surgery to remove the thickened muscle. “This surgery is a one-time thing,” Maron says. Research has found that greater than 90% of people who undergo this surgery have significant improvement of symptoms and enjoy a long-term survival benefit. However, the procedure can be risky if not performed at a top medical institution. In patients for whom open-heart is too dangerous, such as among older seniors, experts may recommend a procedure called an alcohol septal ablation. This involves injecting a small amount of alcohol into the heart, which can shrink the thickened muscle and improve blood flow.
For “a very small number of patients”—and for reasons that are not well understood—Maron says the condition will continue to worsen despite treatment. In these cases, he says a heart transplant may ultimately be necessary.
A positive outlook
While some new medications have helped advance the treatment of hypertrophic cardiomyopathy, experts say improvements in their knowledge of the disease and its clinical management deserve most of the credit for reducing mortality. “When I started 40 years ago, mortality was 6% per year, and treatment was inadequate at best,” Maron says. Nowadays, the annual risk of death for a patient is below 1% percent, his research has estimated.
Experts are also looking ahead to further advancements—and maybe even early interventions that could neutralize the disease before it takes hold. Desai mentions gene editing as, perhaps, the “next frontier” in hypertrophic cardiomyopathy care. “This would involve removing the abnormal piece of genetic material that causes hypertrophic cardiomyopathy,” he says. Gene therapies that aim to replenish certain protein deficiencies are also an area of active research. “If the concept works, in the future patients could walk into the clinic, get an infusion, take immunosuppressants for a few weeks, and potentially be cured or significantly improved,” he says. In the near term, experts are also exploring how the newest medications, if taken early, might be able to reduce or arrest the condition’s progression. “A lot of exciting things are happening in this space,” Desai says.
Hypertrophic cardiomyopathy remains a shifty and unpredictable foe. But experts say they’ve learned to roll with its punches. “Things have moved in the direction we hoped,” Maron says. “This is now a very treatable disease.”
“}]]
Plus, how treatment may evolve.
Uncategorized, freelance, healthscienceclimate
Health – TIME
Plus, how treatment may evolve.
Read moreEnglish News: COVID-Cautious Americans Feel Abandoned
English News: COVID-Cautious Americans Feel Abandoned
[[{“value”:”
For all of 2020, Alex, a 28-year-old living in New York, followed the U.S. Centers for Disease Control and Prevention’s (CDC) COVID-19 guidance “religiously.” Then, in 2021, something began to shift. That spring, the CDC said it was okay for vaccinated people to ditch their masks in most places. But people were clearly still getting sick—including Alex, who got COVID-19 for the first time in late 2021 and later developed Long COVID symptoms.
[time-brightcove not-tgx=”true”]
“There was this reckoning moment where it was like, ‘Maybe the CDC is not being totally honest with us about the situation,’” he says. “‘Maybe they’re trying to present it like we can go back to normal when we can’t.’”
For Alex, who asked to use only his first name to protect his privacy, that feeling has only deepened. The virus killed roughly 1,000 people in the U.S. during the week ending March 2 and has left about 7% of U.S. adults with Long COVID—but despite its continuing toll, real-time data on infections are limited, most mask mandates are gone, and isolation guidance has been scaled back.
The officials making those policies say they are justified, given that almost all of the U.S. population has some immunity to COVID-19, death and hospitalization rates are far lower than they were a few years ago, and tools like rapid tests, antivirals, and updated vaccines are widely available. “We are out of the emergency phase,” CDC Director Dr. Mandy Cohen said in a March interview with TIME. Updated guidelines, such as the end of five-day isolation periods, “reflect that progress,” Cohen said.
But to Alex, it feels less like progress than an attempt to “wrap [the pandemic] up in a pretty bow” and pretend everything is fine. Today, he feels there are “very few” experts he can trust—a sentiment that reflects a growing rift between America’s scientists and the COVID-cautious community, which includes people who are immunocompromised, coping with Long COVID, or simply trying to avoid the virus.
Read More: Experts Can’t Agree If We’re Still In a Pandemic
For much of the pandemic, the scientific establishment and the COVID-cautious public were largely aligned in their desires to contain COVID-19. But as many officials argue for a more moderate approach to living with the virus, COVID-cautious individuals are increasingly the loudest voices calling for continued precautions—and, sometimes, lashing out at the scientists they feel have abandoned the cause.
People who “are still taking COVID precautions seriously have every right to be angry about being abandoned by public-health officials and experts,” says Lucky Tran, a science communicator at Columbia University. “The very real pain that many people are experiencing has not been sufficiently acknowledged.”
Some experts, however, feel they’re in a lose-lose situation, accused of fear mongering one moment and abandoning America’s most vulnerable the next. Experts “feel attacked from all sides,” says Katelyn Jetelina, who writes the popular Your Local Epidemiologist newsletter—and as a result, she fears some will stop trying to communicate at all, further fracturing the already strained relationship between scientists and the public.
Though it may not feel like it, a significant portion of U.S. adults still care about COVID-19. In a KFF survey from late 2023, 26% of respondents said they were “somewhat” or “very” worried about catching the virus, and about half said they planned to take at least one precaution during the winter season, such as wearing a mask or avoiding large gatherings.
Briana Mills, a 31-year-old in California, continues to take many precautions. She has muscular dystrophy and severely decreased lung capacity, which means even a cold could land her in the hospital. With COVID-19 still a threat and with most mitigation measures gone, Mills rarely sees anyone in person except her live-in boyfriend. She ventures out once a month for a park meetup with a group of similarly COVID-cautious people, testing beforehand and wearing a respirator the whole time, but mostly she stays at home.
Mills says she feels abandoned by federal health officials, most recently when they relaxed their COVID-19 isolation guidance in March, even while people like her continue to live in near-total seclusion. “They’re supposed to take care of the people,” she says. “The fact that they’re letting not just disabled people, but people in general, either become disabled or pass away from this virus is very negligent.”
Read More: Long COVID Doesn’t Always Look Like You Think It Does
In certain segments of the population, disappointment with the CDC has been simmering for a long time, to the point that a volunteer group of scientists, health-care workers, public-health experts, educators, and advocates founded a group called People’s CDC to serve as a watchdog and alternate source of information. But federal officials aren’t the only ones drawing ire from those who still take the virus seriously. COVID-cautious Americans are increasingly turning their backs on some of the doctors, epidemiologists, and researchers who built their reputations on helping the public through the pandemic, and are now advocating for more relaxed measures.
Michael Osterholm, director of the Center for Infectious Disease Research and Policy at the University of Minnesota, amassed a dedicated following to his podcast, Osterholm Update, by dissecting COVID-19 policy and talking about his personal precautions throughout the pandemic. Recently, though, Osterholm has loosened up. He no longer wears an N95 mask anytime he goes out in public, since, he says, he’s up-to-date on vaccinations and has access to Paxlovid if he gets sick. And he supports the CDC’s shortened isolation guidelines, arguing they will not meaningfully increase transmission and are more realistic for the average person.
Some listeners have felt betrayed by his loosened stance. “I can no longer, in good faith, be part of this family,” one listener wrote in a note Osterholm read during the podcast’s March 7 episode. “I am so saddened that you are willing to make a mockery of public health and throw a 50-plus-year career down the toilet just to be beholden to the capitalist enterprise.”
Read More: What Happened When a Man Got 217 COVID-19 Shots
Osterholm isn’t overly bothered by the criticism. Listening to and validating people’s feelings is a crucial part of being in public health, he says—and right now, it’s clear that “those who are reluctant to accept the current status of recommendations really do that out of a very real and legitimate personal fear.” The criticism, he thinks, is “less about whatever you say; it’s about whatever they’re feeling.”
Still, while Osterholm is empathetic to those fears, he thinks it’s reasonable and justifiable for COVID-19 policy to change as the virus’ impact on society does. “This is not about abandoning ship,” Osterholm says. “This is about the reality we’re in right now.”
Jetelina, who advises the CDC in addition to writing her newsletter, says she has also struggled to convey that her approach to COVID-19 is evolving with the data, not because she’s stopped caring. She continues to recommend precautions like masking during surges and staying up-to-date on vaccines—but she also argues it’s appropriate to relax a bit now that “we don’t have overwhelmed morgues and we’re not losing 3,500 people a day.”
That message sometimes chafes with longtime readers. In March, Jetelina turned over an edition of her newsletter to someone who has criticized COVID-19 mitigation measures, in an effort to better understand why some people lost trust in public health during the pandemic. Afterward, she got angry emails from followers who felt she was giving a platform to a COVID-19 minimizer. Jetelina has also been accused of downplaying ongoing risks like Long COVID.
It can feel surreal, she says, to get critical messages—and even death threats—from people who feel she isn’t being strict enough in her COVID-19 guidance when, a couple years ago, she was getting bashed for the opposite reason. The never-ending criticism sometimes makes her hesitant to keep publishing the newsletter at all. She recently took several weeks off because she was experiencing stress-related heart issues, and fears other science communicators will give up completely. “A lot of people are just kind of throwing up their hands and moving on, because it’s just not worth it,” she says. “That’s a huge concern of mine.”
Read More: Why Zero Stress Shouldn’t Be Your Goal
Dr. Lara Jirmanus, a clinical instructor at Harvard Medical School and a member of the People’s CDC, has the same fear—that the public will no longer have access to science-backed information—but for a different reason. In her view, many experts have given into “peer pressure” to start moving on from COVID-19, glossing over continued risks like Long COVID; societal inequities that leave some people without reliable access to tests, vaccines, and treatments; and the reality that not everyone is “25 and healthy.”
While there are policy measures that could help make society safer for everyone, such as ventilation standards for public buildings and sick leave policies that allow everyone to stay home when they’re unwell, Jirmanus says independent scientists still have an important role to play. If all experts communicated clearly about the continued risks of the virus, Jirmanus thinks people might be more open to precautions like masking, staying home when sick, and getting vaccinated.
Officials sometimes argue that “public-health guidance is limited by what people are willing to do,” Jirmanus says. “But what people are willing to do is shaped by what experts tell them.”
Data and communication are all Lindy Greer, a 45-year-old in Washington State, wants these days. Greer has taken COVID-19 seriously since the very beginning, both because she previously had long-term symptoms after a non-COVID viral illness and because she works as an esthetician, putting her in close contact with others. She still wears an N95 every day and uses a HEPA air purifier in her work studio, because she still feels COVID-19 is a major threat.
It’s frustrating, Greer says, that many experts, including those she looked up to earlier in the pandemic, don’t seem to feel that way anymore. When even the experts have moved on, she says, it becomes harder for everyone to figure out how to stay safe—and causes people who remain COVID-cautious, like her, to wonder if they’re “crazy” for still caring.
“People in our community are pegged as wanting lockdowns again, and that’s not the case at all,” she says. “All I ever want is for people to have the right information.”
“}]]
There’s a growing rift forming between COVID-19 experts and the COVID-cautious public.
Uncategorized, COVID-19, healthscienceclimate
Health – TIME
There’s a growing rift forming between COVID-19 experts and the COVID-cautious public.
Read moreEnglish News: Japanese Supplement Pill Recalled After Two Deaths and More Than 100 People Hospitalized
English News: Japanese Supplement Pill Recalled After Two Deaths and More Than 100 People Hospitalized
[[{“value”:”
TOKYO — Health supplement products believed to have caused two deaths and sickened more than 100 people have been ordered to be taken off store shelves in Japan.
The products from Kobayashi Pharmaceutical Co., billed as helping to lower cholesterol, contained an ingredient called “benikoji,” a red species of mold.
[time-brightcove not-tgx=”true”]
In addition to the products from Osaka-based Kobayashi, more than 40 products from other companies containing benikoji, including miso paste, crackers and a vinegar dressing, were recalled, starting last week, a government health ministry official said Wednesday.
At least 106 people had been hospitalized, and many more are believed to have been sickened, although it’s unclear if all the illnesses are directly linked to benikoji (pronounced beh-nee-koh-jeeh).
The ministry has put up a list on its official site of all the recalled products, including some that use benikoji for food coloring.
The company is investigating the cause of the problem. The recalled products could be bought without a prescription from a doctor, and could be purchased at drug stores.
Kobayashi apologized and asked in an online statement: “Please stop taking our products, and please do not use them in the future.”
Repeated calls to Kobayashi went unanswered. The company president and other top officials held a news conference last week when the problem first surfaced, bowing their heads in apology, as is the standard in Japan.
The ministry official warned there could be more victims in the days ahead. He asked everyone to stop ingesting anything with benikoji in it. Those with health problems, like weak kidneys, could be especially vulnerable, he said.
All the products were made in Japan, although it is unclear if any of the raw materials were imported. A recall of imported health supplements has happened before, but this is the first major recall of a domestically produced supplement, according to Japanese media reports.
“}]]
Health supplement products believed to have caused two deaths have been ordered to be taken off store shelves in Japan.
Uncategorized, News Desk, wire
Health – TIME
Health supplement products believed to have caused two deaths have been ordered to be taken off store shelves in Japan.
Read moreEnglish News: Living With Muscular Dystrophy at 50 Makes Death My Shadow Partner
English News: Living With Muscular Dystrophy at 50 Makes Death My Shadow Partner
[[{“value”:”
I am an Aries through and through—bold, ambitious, fiery, and confident. Today, March 27, marks my 50th year on this planet, something I could never have imagined. I was diagnosed with an undetermined type of muscular dystrophy as a young child, and doctors told my parents I wouldn’t live to become an adult. My immigrant parents cried when they heard the news. Even though this news was devastating, they never treated me like a fragile egg about to break. In fact, as the first born child of three girls, I had a lot of responsibilities and expectations which only reinforced my Aries tendencies.
[time-brightcove not-tgx=”true”]
While my parents always supported me, I knew at an early age that my life was different. And since they didn’t sugarcoat anything to me, I had a very clear sense that my time was limited. In my bedroom, with a scary clown ceiling light above me at night, my vivid imagination wondered how I would die–would it be a slow and painful death? Would it be fast from a medical emergency? Knowing my muscles are progressively weakening as I struggled to walk as a child and breathe as a teenager always kept death at the forefront of my mind. Believing I had no future shaped me in ways I am still processing today.
Birthdays have given me pause for reflection, especially this year. I recently looked at a picture taken from my 40th birthday party and could not recognize myself. I wasn’t wearing a BiPap mask because at the time I only had to use it intermittently to support my breathing. I did not wear a belt across my chest which I need now because my upper body has grown weaker. I recalled being exhausted after the party. When I got home, I immediately put my mask on and turned on the ventilator. It was a sweet relief. Shortly after I started to use it for longer periods of time until I began using it all day and night. I didn’t see it as a failure of my body but part of the inevitable downward slide toward my final destination.
Two years ago, I experienced the most harrowing and traumatic series of medical crises that led to weeks in the ICU which left me without the ability to speak due to a tracheostomy, a tube in the throat connected to a ventilator, and the ability to swallow and eat or drink by mouth. This resulted in needing a feeding tube that goes into my stomach and intestine. During my hospitalization, I also lost sensation in my bladder so now I urinate through a catheter four to five times a day. Those weeks were like a fever dream–I couldn’t sleep for days because every time I closed my eyes I feared I would never wake up. I was in tremendous pain and could only communicate by mouthing words to my sisters or scrawling on a pad of paper. In the few moments when I could write, I outlined instructions to my sisters on what to do if I didn’t make it. Was this the way I would die? It was my closest brush with death in a series of many but I lived to tell another tale. But I was determined to claw my way forward to another day.
I am still adjusting to life again in a new body and way of life that requires a considerable number of resources, supplies, and machinery to stay alive and avoid institutionalization. The amount of maintenance and administrative work it takes to be disabled in America has also taken a toll—the additional out-of-pocket home care that I need now is $840 a day. With the donations from my GoFundMe dwindling, managing and directing a team of caregivers for my daily activities requires a lot of forethought and clear communication. Being disabled in a nondisabled world is precarious, one of constant adaptation. I remade myself into a new cyborg form that still has a voice, a breath, and a will to live.
Right now, as my body is at its lowest point, I am at the height of my powers. I have never been more happy, free, and resolute on what I want to do. As I turn 50, I am filled with mixed emotions. I dread what lies ahead if I reach 60. Will this be my final decade of life? Maybe it’s ok that I can’t predict what will happen or what the future will hold since no one can. What I will do is spend my time, energy, and labor intentionally with the people I care about. I will host dinner parties, make chili crisp for my friends, and spoil my cats Bert and Ernie. I will treasure every breath pushed through my ventilator and be grateful to have a rare night’s sleep without pain. And most importantly, I will try to rest and care for myself.
Death remains my intimate shadow partner. It has been with me since birth, always hovering close by. I understand one day we will finally waltz together into the ether. I hope when that time comes, I die with the satisfaction of a life well-lived, unapologetic, joyful, and full of love.
“}]]
“As I turn 50, I am filled with mixed emotions. I dread what lies ahead if I reach 60,” writes Alice Wong.
Uncategorized, freelance
Health – TIME
“As I turn 50, I am filled with mixed emotions. I dread what lies ahead if I reach 60,” writes Alice Wong.
Read moreEnglish News: Why Are So Many Young People Getting Cancer? It’s Complicated
English News: Why Are So Many Young People Getting Cancer? It’s Complicated
[[{“value”:”
Just this month, two young, high-profile public figures announced that they have cancer. First, Olivia Munn, 43, disclosed that she was treated for breast cancer after catching it early. Days later, Kate Middleton, 42, announced she has been receiving treatment for an unspecified form of cancer.
[time-brightcove not-tgx=”true”]
Their diagnoses spotlight a troubling trend: both in the U.S. and around the world, cancer diagnoses are growing more common among adults younger than 50. By 2030, one recent study estimated, the number of these early-onset cancer diagnoses could increase by roughly 30% worldwide—and the number of people who die from their conditions could rise by about 20%.
“The most striking finding in the last decade has been this rise in incidence rates among young adults,” says Ahmedin Jemal, senior vice president of surveillance and health equity science at the American Cancer Society (ACS).
Cancer is still most commonly diagnosed among people older than 65. In the U.S., only about 12% of cancers are diagnosed among adults younger than 50, according to ACS data. A woman in the U.S. has about a one in 17 chance of being diagnosed before she turns 50, while a man has about a one in 29 chance, the ACS says. (Women are more likely to be diagnosed largely because breast cancer is so common.)
Read More: The Race to Make a Vaccine for Breast Cancer
But those odds are gradually getting worse. In 2019, about 103 cancers were diagnosed among every 100,000 U.S. adults younger than 50, up from about 100 in 2010, according to a 2023 study in JAMA Network Open. That may seem like a small overall increase, but it’s not a good sign—especially since, during the same period of time, incidence rates among older U.S. adults decreased. “It’s almost like the curves have reversed themselves,” says Dr. Richard Barakat, director of cancer care at Northwell Health in New York.
For certain types of cancer, the numbers are especially striking. Colorectal cancer is now diagnosed among young adults almost twice as often as it was in the 1990s, according to one 2022 study, and the JAMA Network Open researchers found that other types of gastrointestinal cancer are also on the rise among this population. Early-onset breast cancer is becoming more common too, with its incidence rising by almost 4% among U.S. women every year from 2016 to 2019, according to a 2024 study. Even lung cancer, a disease typically associated with older cigarette smokers, is now to a surprising degree affecting younger women, even those who have never smoked, says Dr. Matthew Triplette, a pulmonologist at Fred Hutch Cancer Center in Seattle.
What’s driving these trends? Triplette says he doubts there’s “some new, very dangerous cancer risk factor out there that’s causing tons of excessive cases in younger folks.” Cancer is a complex disease influenced by a mixture of genetics, lifestyle choices, and environmental exposures, so it’s unlikely that there’s a single explanation for the data.
Instead, it’s likely a mix of things. Eating lots of processed foods, not getting enough exercise, and drinking too much alcohol are all risk factors for cancer, and all of those issues are widespread in modern life. A 2019 study co-authored by Jemal found that many of the cancers growing more common among U.S. young adults are linked to obesity, which now affects about 40% of U.S. adults under 40.
Read More: Microplastics in Bottled Water at Least 10 Times Worse Than Once Thought
Researchers are also studying the gut microbiome’s role in cancer development. Everything from what you eat to the medications you take can affect the health of your gut microbiome, Barakat says, so it’s feasible that aspects of the modern diet—or the medical system’s over-reliance on antibiotics—could have trickle-down effects. Exposure to pollutants in the environment could play a role, too, Triplette says.
Even big societal changes could have an impact, Jemal says. For example, research shows that women who give birth to their first child at 35 or younger tend to have a lower risk of breast cancer. In many countries, increasing numbers of women are now choosing to have children later in life or not at all, which could be reflected in cancer rates, Jemal says.
To help lower the risk of cancer, everyone can benefit from evidence-backed health advice like eating a balanced diet, getting plenty of exercise, and not smoking or drinking heavily. But, ultimately, each individual’s chance of getting cancer is different. People with specific risk factors—like genetic markers or a family history of cancer—should consult a doctor about early screening and other preventive measures, Barakat says. Getting a head start can be crucial, he adds, because people with genetic predispositions to cancer are often diagnosed fairly early in life.
It’s also important, Barakat says, to know your body and see a doctor if you think something is wrong. “When I look at some of the patients who were diagnosed with early-onset colorectal cancer, they had symptoms, but nobody thought that a 30-year-old had colon cancer,” he says. The longer it takes to detect cancer, the harder it may be to treat—so it’s important not to assume everything is fine just because you’re young and seemingly healthy.
Of course, every episode of gastrointestinal distress or bloating isn’t a sign of something serious; often, these issues are nothing more than uncomfortable. But if you’re having unusual symptoms that “continue for a long time, you definitely have to look into it,” Barakat says. “And doctors have to be more aware and be a little bit more suspicious.”
“}]]
Kate Middleton and Olivia Munn are part of a troubling trend.
Uncategorized, healthscienceclimate
Health – TIME
Kate Middleton and Olivia Munn are part of a troubling trend.
Read moreEnglish News: Nightshade Vegetables Aren’t Actually Bad for You
English News: Nightshade Vegetables Aren’t Actually Bad for You
[[{“value”:”
If you’ve ever gone down the rabbit hole of health and wellness trends online, you’ve likely stumbled upon the so-called shadowy side of nightshades—vegetables that include tomatoes, potatoes, eggplants, and peppers. What’s made them suddenly newsworthy is that they’ve been singled out by self-proclaimed wellness experts and celebrity dieters as culprits behind a range of health issues, from arthritis to autoimmune disease flare-ups and indigestion.
While there’s little scientific evidence for these claims, some people report feeling better after cutting nightshades from their diets. So before you start side-eyeing your salad, eggplant parmesan, and baked potato, it’s worth taking a closer look.
[time-brightcove not-tgx=”true”]
Why have nightshades become so controversial (and where did that shady name come from, anyway)? Scientists, internal medicine doctors, and registered dietitians shed light on these unfairly maligned vegetables.
What are nightshade vegetables?
Nightshade vegetables come from the Solanaceae family of flowering plants, which are nutritional powerhouses, packed with vitamins (such as C and K), minerals (like potassium and magnesium), and fiber. Dietitians and doctors recommend them in abundance. In fact, they make up a few of the staples in one of the world’s healthiest eating plans, the Mediterranean Diet.
Here’s where the suspicion lies: These vegetables also contain alkaloids, which are natural chemicals produced by plants believed to deter predators. Consumed in very high concentrations, alkaloids, such as solanine in potatoes and eggplants, tomatine in tomatoes, or capsaicin in peppers can cause symptoms such as vomiting, diarrhea, and stomach pain.
This has led to debates about their effects in any dose. Joe Schwarcz, director of McGill University’s Office for Science and Society and author of A Grain of Salt: The Science and Pseudoscience of What We Eat, explains that while nightshades do contain alkaloids, the amount they typically contain are of no consequence. While potatoes, for example, which are eaten by a billion people worldwide, do contain solanine, the amounts are only in traces, he says. An average amount of solanine in a potato’s peel means a 200-pound person would have to eat 20 pounds of potatoes to experience a toxic level, according to the University of Nebraska.
Read More: Why Your Diet Needs More Fermented Pickles
However, there is a higher concentration of alkaloids in green, sprouted potatoes, which is why it’s important to store them in a cool dark place and toss any that have turned green and sprouted. During the 19th century Great Famine in Ireland, people ate a lot of potatoes that had been improperly stored for a long time, says Schwarcz. “But that doesn’t happen in North America. We don’t see potato poisoning or tomato poisoning or eggplant poisoning. We just don’t see it.”
These vegetables also contain lectins, notes Schwarcz, and while lectins can cause indigestion for some people, they’re innocuous for the vast majority.
The name “nightshades” comes in part from the infamous Belladonna plant, also known as the “deadly nightshade,” because it carries a highly toxic alkaloid called atropine, used historically both as a poison and medicine. This connection has stirred up myths about the toxicity of nightshade vegetables. “Just because the tomato and the potato are in the same botanical family as the Belladonna, it doesn’t mean that they are equally poisonous,” Schwarcz says.
The Tik-Tok effect: claims vs. science
On social media, you’ll find no shortage of videos and blogs vilifying nightshade vegetables, with titles ranging from “Foods to avoid if your pup suffers from arthritis,” to “These veggies could be worsening your eczema!” Most are the work of influencers and “self-appointed nutritional gurus,” notes Schwarcz. In his opinion, these creators run the gamut from “total incompetence…to physicians who have gone astray.” There are also many testimonials from people with autoimmune conditions such as lupus, psoriasis, and inflammatory bowel disease (IBD) who swear that they feel better when they cut out nightshades. While medical and nutrition experts suggest that some people likely would benefit from an elimination diet, blanket warnings against nightshades aren’t warranted.
Dr. Rebecca Kuang, an internal medicine resident at the University of Pittsburgh Medical Center, has been studying the connection between nightshades and gastrointestinal diseases. A literature review she co-authored last year showed that the natural chemicals in these vegetables might disrupt the gut barrier and possibly worsen symptoms for those with certain bowel diseases such as IBD. Many of the studies in the review were in mice, but if the findings hold true for humans, eating too many of these vegetables may worsen symptoms for those with certain bowel diseases such as IBD.
Read More: Why You Suddenly Have Allergies
Nightshades also contain potential allergens that might cause reactions similar to other food allergies, with cross-reactivity between foods in the nightshade family and others. Kuang’s research shows there is potential for nightshades to trigger mast cell activation, leading to inflammation and discomfort in the GI tract, similar to an allergic reaction.
However, research in this area is still new, with many studies relying on animals or involving variables that could affect the results. For example, Kuang is interested in how a nightshade vegetable’s preparation—such as fried potatoes with a high fat content—could affect some of the alkaloid levels. More basic science and human studies are needed, she says, to fully understand how nightshade foods may irritate the GI tract.
“I wouldn’t want the takeaway to be that everybody should be avoiding these foods,” she says, “but certain people might have sensitivities to them.”
What to do if you suspect you have an intolerance or allergy to nightshade vegetables
Navigating the complicated issues of food sensitivities, allergies, and intolerances can be tricky, particularly when it comes to nightshades. Diet and nutrition experts stress the importance of personalized approaches rather than broad exclusions. Lona Sandon, an associate professor in the department of clinical nutrition at the University of Texas Southwestern Medical Center, brings a personal perspective to her professional insights, having lived with rheumatoid arthritis, an autoimmune condition, for 30 years. “It’s been a long-standing folklore,” she says, adding that she’s tried eliminating nightshades herself, along with many other foods—to no avail. “There was not enough fish oil in the world, not enough fruits and vegetables in the world, that was going to fix what was happening with my immune system,” she says. Despite decades of debate, evidence about the nutritional impact of nightshades hasn’t increased much. “In fact,” Sandon says, “there’s more research to support that people should be including these foods in their diet when they have inflammatory conditions such as rheumatoid arthritis.”
If you suspect you may be sensitive to nightshades, Sandon says, don’t eat them for two weeks. Then slowly introduce them back into your diet. Allow about three days between each one, as reactions can be delayed. She recommends keeping a food and symptom diary to track potential sensitivities.
Read More: Magnesium Supplements Are a Buzzy New Sleep and Anxiety Aid. Do They Work?
Briana Butler, CEO of Gnaw Collective and a registered dietitian nutritionist specializing in nutrition coaching for athletes and women of color, explains that a registered dietitian can guide individuals through an elimination diet to identify food sensitivities and examine other potential factors like gut health. “There just is not enough research, in my opinion, to just cut [nightshades] out completely,” she says. “Those statements cannot possibly apply to everyone. It literally has to be a case-by-case basis and figuring out okay, what is actually going on?”
Butler points out that outright allergies to nightshades are rare, as they aren’t in the top nine most common allergens. Both Sandon and Butler caution against eliminating nightshades without substantial evidence of personal sensitivity. They encourage consultation with health care professionals for those experiencing adverse reactions, to ensure dietary changes are both necessary and beneficial.
The biggest takeaway? Our bodies react in unique ways to different foods. While some people might need to steer clear of certain foods, labeling them as toxic for everyone misrepresents the complexity of human biochemistry, says Schwarcz. “The main problem here, as with so many such issues, is taking a kernel of truth and then extrapolating it.” He cautions against the broad brush of fear-mongering on platforms like TikTok, where personal sensitivities are sometimes inflated into universal truths. Above all, most Americans don’t eat enough fruits and vegetables to begin with. Why limit your choices even further?
“Some people can’t tolerate beans or eggplants or whatever. You don’t eat them. But you don’t go on TikTok and tell everyone in the world that this is a poison,” he says. Schwarcz, for instance, is allergic to fish. But fish is healthy—and he’d never tell you to steer clear of it just because he does.
“}]]
Influencers love to malign tomatoes, potatoes, eggplants, and peppers.
Uncategorized, Evergreen, freelance, healthscienceclimate
Health – TIME
Influencers love to malign tomatoes, potatoes, eggplants, and peppers.
Read moreEnglish News: How to Safely Watch the Total Eclipse
English News: How to Safely Watch the Total Eclipse
[[{“value”:”
The first solar eclipse I had a chance to witness I in fact didn’t witness at all. It was July 20, 1963, and I was attending Camp Comet in Waynesboro, Pa. The camp’s owners and counselors—not to mention, our parents—wanted nothing to do with the prospect of 150 literally wide-eyed boys staring directly at the sun as the moon partly obscured it. So they kept us inside our geodesic-dome-shaped bunks and draped blankets over the windows until the danger had passed.
[time-brightcove not-tgx=”true”]
From a safety perspective, that, in fact, was not a bad precaution. That’s because there is a lot of damage the sun can do to the retina of the eye as the eclipse approaches and then passes totality—and that damage can affect your vision for life. So, if you’d like to bear witness to a celestial event that will not touch the U.S. mainland again until Aug. 23, 2044, while at the same time protecting your eyes and preserving your sight, here’s how best to observe the upcoming April 8 total eclipse.
What looking at the eclipse does to your eyes
The good news is that the most transcendent and transformative part of a total solar eclipse takes place in the relatively brief period of totality, when the disk of the moon is completely covering the disk of the sun. During these few minutes it’s safe to look up with unprotected eyes and take it all in. The bad news is that matter of brevity: The longest the April 8 eclipse will last as the path of totality tracks from Texas to New England will be just shy of four and a half minutes, over portions of Texas. In other cities the duration of totality will be less than that. But the hours that will unfold before and after that moment, when the sun is first reduced to a steadily shrinking crescent and then reappears as a growing one, are perilous.
The reason is that while your surroundings may get darker during the slow disappearance of the sun, looking directly at light caused by a solar crescent is no safer than looking at the sun at any other time—and the squinting and blinking you’ll do if you try are your eyes’ reflexive way of protecting you from the damage you’re doing to them. As the Cleveland Clinic explains, the lens of your eye operates like any other lens, concentrating incoming light to a hot and fine beam. Much like using a magnifying glass’s lens to burn a piece of paper or wood, the retina of the eye can similarly be burned, causing damage and scarring.
Read More: How Animals and Nature React to an Eclipse
“Solar retinopathy is a photochemical injury to your retina,” wrote Dr. Nicole Bajic, a surgical ophthalmologist at the Cleveland Clinic, in an email to TIME. Unstable molecules from the sun, called free radicals, damage both the pigment of the retina and light-sensitive photoreceptor cells, she explains.
Worse, as with anything you’re concentrating on visually, you’ll almost certainly be focusing that incoming solar energy on the central part of the retina, known as the macula, which is the part that processes fine detail. When you’re reading, you’re using your macula; when you’re identifying faces, you’re using your macula; when you’re making subtle distinctions among colors, you’re using your macula. Fry that part of the eye, and you’re destroying the most valuable real estate your retina has.
The popular idea, or at least the popular fear, is that eclipse-related retinal damage will lead to blindness—and the fact is, if you look long enough and the retina is burned severely enough, the eye could indeed grow entirely dark. However, in most cases, the harm that’s done will lead to blurred vision, floaters, blind spots, or so-called low vision—similar to trying to see in a darkened room. Bajic warns that blind spots or decreased vision “unfortunately can be permanent in some cases.”
What’s true for looking at a partially obscured sun with your naked eye is true too of looking at it through a telescope, camera, binoculars, or even through your phone. And forget about sunglasses; they don’t screen out nearly enough light to keep you safe.
Buy the right eclipse glasses
What does work, as NASA and the American Astronomical Society (AAS) recommend, are hyper-shaded, eclipse-rated glasses with lenses that carry the ISO 12312-2 darkness rating. Glasses without that designation will not protect your eyes sufficiently, even if you don’t feel like you’re getting too much light.
Read More: How Cities Around the U.S. Are Celebrating the Eclipse
However, there are counterfeit eclipse glasses out there, and trying to buy protection on the cheap can carry a very high long-term price. It’s thus best to purchase glasses only from reputable marketers. The AAS has a Suppliers of Safe Solar Viewers & Filters page on which it lists what it considers to be reliable sellers not just of glasses, but of safe filters for telescopes, binoculars, and cameras as well.
Make a viewing box
Another method for viewing the sun before totality—or at least a simulacrum of the sun—is to make a pinhole projector simply by poking a hole in a piece of paper or cardboard, holding it in the path of the sun, and looking down at the ground or any other surface, rather than up at the sun. The point of light that comes through the hole will instead be a crescent, precisely capturing the amount of the sun that is missing at the moment you view it. A colander can achieve the same effect, and in this case will produce a whole spangle of crescents. As I learned to my surpassing delight during the May 10, 1994 partial eclipse, when I hastened over from my office to the leafy southeast corner of Central Park in New York, merely standing under a tree will allow you to see the dappling of light that passes through branches as a dappling of crescents on the ground.
Ultimately, 35 years after I missed my first shot at a total eclipse, I did at last catch up with one, aboard a ship just to the west of the Panama Canal, on Feb. 26, 1998. As the skies darkened and the waves lapped, a corona of solar flames seemed to explode from behind the black disk of the moon. I had guarded my eyes in 1963, and the span of three and a half decades that passed before I at last beheld an eclipse—safely viewing it through eclipse glasses—was well worth the wait.
“}]]
The total eclipse on April 8 will be a magnificent spectacle. Here’s how to protect your eyes.
Uncategorized, Eclipse, healthscienceclimate
Health – TIME
The total eclipse on April 8 will be a magnificent spectacle. Here’s how to protect your eyes.
Read moreEnglish News: Puerto Rico Declares Public Health Emergency as Dengue Cases Rise
English News: Puerto Rico Declares Public Health Emergency as Dengue Cases Rise
[[{“value”:”
Puerto Rico declared a public health emergency over dengue, a mosquito-borne illness that has surged throughout the Americas this year.
Read More: Dengue Fever Is Soaring Worldwide. Here’s What to Know—and How to Stay Protected
Health officials in Puerto Rico have identified 549 cases of dengue across the U.S. territory of 3.2 million people, with almost half the cases concentrated in the capital of San Juan. Also known as “breakbone fever,” dengue can cause headaches, soreness, fever and rashes—and, in extreme cases, death.
“This year, cases of dengue have surpassed historical records,” Health Secretary Carlos Mellado said in a statement.
The emergency declaration has no immediate impact on travel to or from Puerto Rico, a popular holiday destination, but it will make it easier for the health department to access funding for detection and prevention, Mellado said.
There have been major outbreaks of dengue this year across large swathes of the Americas, including Argentina, Uruguay, Brazil and Peru. Last year, parts of Florida were put under a mosquito-borne illness alert due to dengue.
“}]]
Puerto Rico’s dengue emergency has no immediate impact on travel but will make it easier for the health department to access funding for detection and prevention.
Uncategorized, News Desk, overnight, wire
Health – TIME
Puerto Rico’s dengue emergency has no immediate impact on travel but will make it easier for the health department to access funding for detection and prevention.
Read moreEnglish News: There’s a Reason They’re Called ‘Gut’ Feelings
English News: There’s a Reason They’re Called ‘Gut’ Feelings
[[{“value”:”
In the 1800s, a French Canadian named Alexis St. Martin was shot in the stomach while at a fur trading post, when someone’s musket accidentally fired at close range. He survived, but his injuries resulted in a hole in his stomach wall. This provided an early window—literally—into how our emotions and mental health affect the gut. Through careful experiments, the surgeon William Beaumont discovered that St. Martin’s mental state had direct physiological consequences on his stomach’s activity: when he felt irritable, for example, his digestion slowed. Somehow, his emotional states were manifest in the specific, local biology of his gut.
[time-brightcove not-tgx=”true”]
Most people have experienced the gut consequences of their emotional feelings. Nerves before an exam might lead you to feel nauseous or even vomit. Profound sadness might make you lose your appetite, or perhaps cause a hunger impossible to satiate. Gut symptoms are common in mental health conditions, from appetite changes in depression to debilitating “psychosomatic” stomach pains. Many of our feelings are gut feelings.
But the gut doesn’t just respond to emotional feelings: it influences them, too. Take disgust. Disgust is visceral. Our stomach, like our heart, has a regular electrical rhythm; even just seeing something disgusting causes disruptions, called “dysrhythmias,” in this electrical signalling. Although disgust is crucial for survival—helping us avoid disease and stay alive—in many mental health conditions disgust becomes pathological. In obsessive compulsive disorder (OCD), for instance, dirt or germs can preoccupy someone’s thoughts, causing symptoms like compulsive hand-washing. Self-disgust is common in depression and eating disorders. And even post-traumatic disorder can be brought on by profoundly disgusting traumas.
Pathological disgust is particularly hard to treat: exposure therapy and other psychological approaches are much less effective than for fear-based mental health problems. A couple years ago, working as a neuroscientist at the University of Cambridge, I wondered if abnormal signals from the stomach could be causing disgust avoidance. I ran an experiment to test this hypothesis, and found that changing someone’s gut activity with a common anti-nausea drug reduced their disgust avoidance. This could represent a new way of treating pathological disgust in mental health disorders. For example, an anti-nausea drug could be administered just before exposure therapy, enabling patients to engage with therapy under a more optimal gut state.
Read More: How I Learned to Listen to What My Gut Was Telling Me
So gut feelings are not “all in your mind”—but they are not “all in your gut,” either. Sensations from the gut are transmitted to the brain via the vagus nerve, the primary channel of information sent from the body to the brain. A second route to target “gut feelings” is by electrically stimulating this nerve, which changes the electrical rhythm of the stomach. That said, the idea is not new: vagus nerve stimulation for patients with major depression dates back to 2000.
A new theory published in November 2023 proposes that vagus nerve stimulation amplifies signals from the internal body to the brain, which helps us adapt our behaviour to its current challenges and needs. That could explain why the effects of vagus nerve stimulation are so wide-reaching, altering learning, memory, and motivation. That means amplifying signals from the gut using vagus nerve stimulation might improve mental health in some cases, but in others could be ineffective or even detrimental. Ultimately, we need to consider the state and needs of someone’s internal body before amplifying the body’s influence on the brain.
But the importance of the vagus nerve extends to even more established treatments: evidence from mice suggests that the most common type of antidepressant drugs (SSRIs, or selective serotonin reuptake inhibitors) require the vagus nerve to work. This, too, could begin to provide clues why antidepressants do, or don’t, work for a given person, and even help us understand why they might cause side effects in some people.
If the vagus nerve’s role helps us adapt to our bodily needs, perhaps the most important internal need of all is energy. One function of the gut—together with other organs—is metabolism, converting food to energy the body can use. There are mysterious and wide-ranging connections between our metabolic system and mental health. For example, the prevalence of depression in people with diabetes is two or three times higher than in the general population. It’s not clear why: diabetes could increase depression risk, or vice versa. My lab is currently testing a third possibility: that common metabolic factors might increase your risk of both depression and diabetes because of interactions between the body and the brain. If we’re right, this could open up avenues toward metabolic interventions that improve both physical and mental health.
Our brain and wider nervous system adapts to its circumstances, including the body’s internal, metabolic needs, as well as our experience of the environment around us. Because of this, your gut-brain connection is not static, but rather changes and adapts over time. A fascinating study in 2021 discovered that brain cells can re-activate gut inflammation that an animal has previously experienced. The mere “memory” of gut inflammation, stored in cells in the brain, induced the physical state in the body. So sometimes a “gut feeling” actually originates from the brain. This role of the brain in “gut feelings” means our brain has the capacity to produce dysfunctional gut symptoms via brain changes alone. This ability of the brain could have upsides as well, perhaps explaining why psychological therapy—which causes brain changes—can also treat some gut conditions.
Gut feelings originate from many sources: directly through the gut, through channels of communication between gut and brain, or even through the brain itself. In neuroscience, as we unravel the dynamic communications between gut and brain, we can begin to understand how these processes helped our ancestors survive—and how we could better harness them to improve emotional and mental wellbeing. A gut feeling might have many possible causes, but each of these represent a potential solution for mental health.
“}]]
Neuroscientist Camilla Nord explores how the gut doesn’t just respond to emotional feelings. It influences them, too.
Uncategorized, freelance
Health – TIME
Neuroscientist Camilla Nord explores how the gut doesn’t just respond to emotional feelings. It influences them, too.
Read moreEnglish News: Are Personality Tests Actually Useful?
English News: Are Personality Tests Actually Useful?
[[{“value”:”
Ask Erin Mantz why she loves personality tests, and she’ll tell you she’s a Pisces, an only child, and an introvert prone to self-reflection. “I’m constantly craving and searching for insights into why I do what I do, and what makes me tick,” she says. Since discovering them at her college career center, she’s taken many different kinds, but the most transformative was the one she took with her coworkers at AOL in her 30s. A new manager instructed Mantz and her colleagues to take the Myers-Briggs Type Indicator test, which revealed she’s an INFJ: intuitive, enthusiastic, impulsive, and prone to improvisation.
[time-brightcove not-tgx=”true”]
The test changed the whole vibe of the office. “We all shared our results and kept a Post-it on our desk with what everybody’s type was,” Mantz recalls. “Then when Frank called or you needed to present information to Aaron, you’d understand where they were coming from or how to best get through to them.” Some people preferred to hear about potential impact, for example, while others responded best to hard facts. The knowledge has proven useful in her personal life and throughout her career, she says, helping her figure out how to better communicate with others and make the best impression.
Personality tests aren’t new—an early version of the Myers-Briggs test was copyrighted in 1943—but interest in them has endured. People slap their four-letter Myers-Briggs type on their dating profiles and broadcast their Hogwarts House at parties. Many use the results to figure out what career paths might appeal, and some companies use them to decide who to hire.
But why do people like personality tests so much, and which are the most accurate? How should—and shouldn’t—we interpret their results?
Personality tests make you feel seen
Personality tests are a useful way for people to better understand themselves, especially when they’re young, says Brent Roberts, a professor of psychology at the University of Illinois Urbana-Champaign who studies personality development and assessment. “We’re trying to figure out ourselves and why the world reacts to us the way it does,” he says. “I think everybody wants to better know who they are, and where they stand—and that’s what a personality test can give you.”
Ashley Errico, a therapist in Austin, remembers buying All About You! magazine as a pre-teen, drawn to the cover-to-cover personality tests. She and her best friend would listen to the Spice Girls while taking tests to find out what kind of kisser they’d be. Now, in her professional career, she sometimes directs clients to more sophisticated tests, like the Myers-Briggs (which costs about $60 to take online) and Enneagram. (The latter, which costs $20 online, sorts people into one of nine personality types, such as “achiever,” “helper,” or “challenger.”)
Read More: The Psychology of Why We Get ‘the Ick’
Errico has found that the Myers-Briggs test, for example, can supply people who want to change careers or return to the workforce with some ideas that hadn’t been on their radar. There’s a paid service that matches personality type to jobs that might be a fit, and some career counselors are trained to provide feedback. (You can also just Google “jobs for INFJ,” for instance.) “I’ll say, ‘Use those as a starting point, because it might suggest things you’d enjoy but never think about,’” Errico says. Plus, personality tests foster a sense of recognition and belongingness. “Everybody wants to feel understood and seen,” she says. “We all know what it’s like to feel invisible.”
But they really oversimplify things
Personality exists on a spectrum, and no single test can capture all the nuances that define a person. Tests like the Myers-Briggs and Enneagram “aren’t able to describe the richness of human diversity,” says Jaime Lane Derringer, a scientist at the University of Illinois Urbana-Champaign who works at the intersection of personality psychology and molecular genetics.
Take the Myers-Briggs: It distills a person’s traits into 16 different personality types, such as ESFJ (extrovert, loyal) or ENTP (extrovert, imaginative). There are more personality types than that, Derringer says. Plus, the tool frames personalities around positivity—omitting more negative traits, like neuroticism or not being conscientious. “It’s a great marketing machine,” she acknowledges—people love hearing the good parts about themselves—but certainly not comprehensive.
Many personality tests use generic language in their results that could easily apply to whoever is reading it. Scientists call it the Barnum Effect. “It comes from P. T. Barnum saying there’s a sucker born every minute,” says Stephen Benning, a psychology professor at the University of Nevada Las Vegas who studies basic emotional processes. “They’ll basically be able to take this very generic statement about universal human tendencies and somehow think it’s uniquely applicable to them.” That, he jokes, is why there are three things his students can do that make him bang his head on his desk: ask him his Enneagram, his Myers-Briggs type, or his horoscope.
Read More: How to Start Foraging, According to TikTokers
One of the risks associated with personality tests, Roberts believes, “is taking the information too seriously.” These tests are based on self-reported data—it’s up to you to gauge how often you feel angry or excited, and whether you tend to find fault with others. That’s not always accurate. “There are places in our psyche that we’re blind to and might not quite understand,” Roberts says. “Just relying on what you think about yourself is an error, in my estimate.” It’s better to seek out more information from a variety of sources, he says—which could include working with a mental-health professional.
Errico cautions her therapy clients not to over-identify with their results. She’s seen people get too invested in their personality type, which prevents them from allowing themselves to grow and change. Or, they might push themselves into a job that’s not the right fit, because their personality test indicates they should enjoy it. “It’s important to remember that the test doesn’t determine who we are,” she says. “We get to determine who we are.”
Which personality tests are best?
Free online tests that tell you what wild animal or cake you are might be fun, but that’s all they are: entertainment. Some personality tests, however, have been studied for decades, and researchers have a solid sense of their pros and cons. The academic community generally considers tests based on the Big Five to be the most scientifically rigorous. It’s a nearly 75-year-old model developed to measure five broad personality traits—conscientiousness, agreeableness, neuroticism, openness, and extraversion—and lots of free online tests are based on it. “It’s well-replicated across samples, across nations, across time,” Benning says. Taking one of these tests can help people broadly understand their individual differences in personality, and how their tendencies might influence the ways that other people perceive them.
Roberts often directs his students to O*NET, a free U.S. Department of Labor online test that matches users’ interests and level of work experience to potential careers. “It tells you, ‘Here are all the jobs where you’d be more likely to be happy and satisfied,’” he says. “It’s a beautiful tool.” Another free test, the RIASEC model, can similarly help people assess occupation interests. It helps respondents understand if they have, for example, investigative, artistic, social, or enterprising personalities.
Read More: How to Respond to an Insult, According to Therapists
Mental-health clinicians sometimes administer the Minnesota Multiphasic Personality Inventory (MNPI), says Dr. Rehan Aziz, an associate professor of psychiatry and neurology at the Hackensack Meridian School of Medicine. It consists of nearly 600 true-false questions that can help reveal mental-health conditions such as hypochondria, depression, and paranoia. “It’s a very lengthy test, but I found that it gives really accurate results,” he says. “It has internal validity measures, which a lot of these personality tests don’t have—which means it can tell if you’re giving inconsistent or inaccurate answers, or if you’re trying to ‘beat the test.’” If you’re interested in learning more about the MNPI, which isn’t available online, bring it up with your psychologist, Aziz advises.
Whichever test you take, consider repeating it every once in a while. Much of Roberts’ research focuses on the ways personality changes over time: Most people shed some of their neuroticism as they age, he notes, and people also tend to get more conscientious as they grow older. “It’s totally useful to come back in a few years and take the test again to see where you’re at,” he says.
And, most importantly, don’t attach too much significance to any personality test-generated label. “None of them are perfect—they’ve all got flaws, and they’ve all got strengths,” Derringer says. “They can’t tell you who you are, but they can provide a framework for you to begin to introspect, and a way to anchor yourself in comparison to other people.”
“}]]
They can aid introspection—but experts warn against taking the results too seriously.
Uncategorized, Evergreen, healthscienceclimate
Health – TIME
They can aid introspection—but experts warn against taking the results too seriously.
Read moreEnglish News: Kate Middleton Is Receiving Preventative Chemotherapy. Here’s What That Is
English News: Kate Middleton Is Receiving Preventative Chemotherapy. Here’s What That Is
[[{“value”:”
In a video released by Kensington Palace, Kate Middleton revealed why she has been out of the public eye for months: she was diagnosed with cancer and has been receiving preventative chemotherapy. She did not say what type of cancer she has or the stage of her disease, but she began receiving preventative chemotherapy in late February, according to a statement from Kensington Palace.
[time-brightcove not-tgx=”true”]
“In January, I underwent major abdominal surgery in London and at the time, it was thought that my condition was non-cancerous,” the Princess of Wales said in the video. “The surgery was successful. However, tests after the operation found cancer had been present.”
“My medical team therefore advised that I should undergo a course of preventative chemotherapy and I am now in the early stages of that treatment.”
What is preventative chemotherapy?
Doctors say preventative chemotherapy can refer to a wide variety of medicines for many different types of cancer. It’s not a medical term, but the Princess of Wales is most likely referring to what doctors call adjuvant chemotherapy, which usually involves the same chemotherapy drugs that people receive to treat advanced cancer. It’s meant to kill any remaining, microscopic cancer cells a surgeon could not see and may have missed, and to destroy any cells that may have escaped and spread to other parts of the body.
Read More: The Race to Make a Vaccine for Breast Cancer
Depending on the type of cancer, studies have shown that giving “anywhere from three to six months of chemotherapy after surgery can significantly reduce the risk of cancer coming back,” says Dr. Jeremy Jones, interim chair of the division of hematology and oncology at the Mayo Clinic, who has no personal knowledge of Kate’s case. “It’s standard of care to reduce the risk of recurrence for many types of cancer.”
Jones says doctors decide to start adjuvant chemotherapy based on a combination of factors, but the main criterion is the stage of cancer. Cancer stages take into account whether cancer cells have spread to lymph nodes or other parts of the body, so adjuvant chemotherapy is mostly recommended for later-stage cancers that have a higher risk of recurring, he says.
How is preventive chemotherapy different from regular chemo?
When all visible traces of a patient’s cancer have been removed during surgery and adjuvant chemotherapy is used, doctors can prescribe any of the hundreds of agents that are available to treat more advanced cancers. Sometimes these are given in lower doses, but often they’re administered in the same doses as those used for treating cancer, says Jones.
However, people who receive adjuvant chemotherapy may only need short courses compared to those getting chemotherapy to treat more serious disease, says Dr. Beth Karlan, director of women’s health research at UCLA’s Jonsson Comprehensive Cancer Center. Most of the time, the drugs are delivered via infusion at a hospital or facility over the span of a few hours, but some may require more time; those patients may receive a port and return home with a pump that continuously provides the chemotherapy over a day or so. Most courses of preventive chemotherapy last at least three months.
“There is a lot of evidence to support adjuvant chemotherapy impacting overall survival, and allowing patients to live years longer and perhaps even effecting a cure,” says Karlan. The hope is that “it is preventing recurrence and thereby allowing her to live a full and productive life. The example she is providing with her message will have a salutary effect on so many other people.”
“}]]
The Princess of Wales revealed she is taking preventive chemotherapy. The treatment is commonly used after surgery when cancer is present.
Uncategorized, healthscienceclimate
Health – TIME
The Princess of Wales revealed she is taking preventive chemotherapy. The treatment is commonly used after surgery when cancer is present.
Read moreEnglish News: How to Manage Anxiety and Depression When You Have Kidney Cancer
English News: How to Manage Anxiety and Depression When You Have Kidney Cancer
[[{“value”:”
When Katie Coleman was diagnosed at age 29 with a softball-sized tumor on her right kidney and a host of smaller growths in her liver, she was stunned. That astonishment quickly gave way to feelings of hopelessness. “I felt like my entire world was being pulled out from under me,” Coleman, now 32, says. “I went into a very dark spiral.”
Though her surgeon removed all the tumors, it wasn’t clear what her long- or even short- term prognosis was. What she found on the internet just freaked her out more. “One night I spiraled so deep I didn’t know whether life was worth living anymore.”
[time-brightcove not-tgx=”true”]
Coleman knew she needed help dealing with her depression and anxiety, but she didn’t form a strong connection with any of the therapists she met with. “I never found one who really understood what it was like to be 29 and looking fate in the face,” the software engineer from Austin says.
At her darkest point, Coleman started browsing Instagram posts, “looking for anyone who had what I had,” she remembers. “I needed to see someone else who was still alive.”
She eventually found a match, a man in the U.K. She wrote to him: “I’m sorry to be a random stranger on the internet. I was hoping you would share your story.”
The next morning, she discovered a stream of voice memos from someone with a British accent. “First, you need to get the idea of dying out of your mind,” the voice said.
“He told me how full of a life he felt he was living,” Coleman says. “It was the first time I connected with another patient and the amount of hope it brought me is indescribable.”
Coleman started putting together her own internet-based support group. “Folks pulled me out of some very dark places,” she says. “I always had someone to go to to talk things over.”
The value of short-term goals
The National Cancer Institute estimates that there were nearly 82,000 new kidney cancer diagnoses in 2023. Anywhere from 10% to 50% develop symptoms of anxiety and/or depression after diagnosis, experts say.
Because of that, many cancer centers have added psychiatrists, psychologists, and counselors to their treatment teams. “Anxiety and depression are common complications in oncology,” says Dr. Jon Levenson, an associate professor of psychiatry at the Columbia University Vagelos College of Physicians and Surgeons. “One major stressor is the uncertainty about the course their cancer will take. Patients may have surgery to remove the cancer and be physically asymptomatic for many months, or even longer, but still know there’s a high likelihood of recurrence.”
The stress from all that uncertainty can ramp up to full blown depression and/or anxiety, Levenson says.
For Coleman, the uncertainty was initially paralyzing. “At 29, I was very ambitious,” she says. “I was used to setting long-term goals. Now I didn’t know what next week would look like.”
But Coleman found a way to cope. She started to concentrate on short-term goals—small ones that she could accomplish in the three months between scans. Early on she set a goal of designing a health records app that could help others with cancer keep track of their care. She accomplished that in one of the three-month periods between scans. As time went on and her scans remained clear, Coleman decided to take a chance and started writing a memoir.
Read More: 7 Myths About Kidney Cancer, Debunked
Talking helps—but don’t share everything with everyone
Support groups of any kind can make a person with cancer feel less alone, says Shannon La Cava, director of the Simms-Mann/UCLA Health Center for Integrative Oncology. Sometimes patients say they don’t want to attend a support group, but “I say try two or three sessions,” she adds. “A lot of times after dipping a toe in people say ‘Oh wow, finding people like me gave me a lot of support.’”
That doesn’t mean patients need to share everything with everyone.
Patients often struggle with questions of “who to tell, when to tell, and what to tell,” says Dr. Asher Aladjem, medical director of psychological services at the NYU Langone Perlmutter Cancer Center. “If it makes a patient more anxious to have everybody involved in their experience, I advise them to be very selective about who to tell. I tell patients, ‘Pick a small group of people to tell and choose how much detail you want to give.’”
Aladjem says he tries to help patients draw boundaries and stick with them. In some cases, that may mean telling people you’d rather talk about something enjoyable, like movies.
It’s important, Aladjem says, for patients “to maintain control over what their experience is. There’s already a sense of loss of control with the illness. I think empowerment is very important.”
On the other end of the spectrum, some patients don’t want to talk to anyone.
When Travis Ferguson was diagnosed with kidney cancer at age 40, he kept everything to himself. While he felt empowered enough to leave the medical center in Indiana where he was diagnosed to seek care at a center that specialized in cancer, Fox Chase Cancer Center in Philadelphia, he didn’t know what to do with his fears, anxiety, and depression.
“When I first found out, I went into a real depressive state because I have two grandparents who died from cancer,” he remembers. “It felt like a death sentence. I thought talking about it would make it even more real.”
Although Ferguson had a therapist he’d been seeing to figure out how to deal with some other big life changes, including a recent breakup with his girlfriend, he initially didn’t bring up cancer during their sessions. “I finally brought it up with her because I realized I needed help,” he says. “I had been sliding deeper and deeper into the abyss.”
The therapist increased the dosages of the anxiety and depression medications he was already taking. Then she pushed him to start talking to his family. “They helped tremendously,” says Ferguson, now 41.
Read More: The Latest Breakthroughs That Could Improve Kidney Cancer Treatment
Who am I now?
As Jay Wells knows, the diagnosis can steal a patient’s sense of self. He’d been a park ranger for 30 years and saw himself as a rescuer of others until he was diagnosed with advanced kidney cancer at 68.
“I went from feeling strong and invincible to weak and fragile overnight,” says Wells, now 72. “I had been in a profession that was counted on to go in and rescue people in a bind, after a climbing accident or falling into a river. Now the roles were reversed. Everything was out of my control. It was a hard adjustment.”
Wells started worrying about dying and how his death would impact his wife. “She couldn’t take care of the house and 11 acres alone,” he says. “And who was going to take care of my dog?”
Depression and anxiety set in. At first, Wells resisted going to see a therapist. Then, “I started showing signs of depression,” he remembers. “I’d start thinking about stuff, and sometimes I’d break out crying in front of my wife, and even good friends. They could see I was in emotional pain.”
Eventually, Wells took the advice of those who loved him. He found a therapist who specialized in treating patients with cancer. “She suggested a bunch of things that helped, like meditation and breathing exercises to calm my anxiety. She had me do exercises where I would write about my fears of dying, what I was leaving undone, who I would leave behind, and how I would want to be remembered.”
The writing and conversations with the therapist made a big difference. “It was a way of getting at the anxiety and fears that were lurking just below the surface,” says Wells, who now lives in Ashland, Oregon. “Though it seemed like every time emotions were evoked that choked me up, I felt so much better afterwards.”
A kidney cancer diagnosis often comes as a shock because there haven’t been any obvious symptoms, says Dr. George Schade, a surgeon, associate professor at the University of Washington, and physician with the Fred Hutchinson Cancer Center in Seattle. So it shouldn’t be a surprise that many are shaken by it, he says, adding that some 70% to 80% of patients experience symptoms of anxiety and/or depression.
Those who need help with their emotional distress are generally referred to in-house team members, Schade says. But many patients don’t live close enough for weekly or biweekly appointments. “Patients might be five minutes away or from Alaska or Montana,” Schade says. “So telemedicine has been a huge game changer for us.”
Not every cancer center has mental health professionals on their teams, which means patients need to seek help in their local community, says Dr. Rafael Tamargo, an assistant professor in the department of psychiatry and behavioral sciences at Vanderbilt University Medical Center.
Unfortunately, there is a nationwide shortage of people in these professions now.
While patients look for someone, Tamargo recommends a few self-help methods—such as breathing techniques—to calm anxiety and soothe depression. For example, he suggests an exercise where one breathes slowly through the nose for four seconds, then holds their breath for four, then exhales through the mouth for four, and then waits another four before repeating.
Another way to calm down, he says, is to lie on your back with your eyes closed on a flat surface with your legs and arms extended. Then starting with your toes and working up to your head, focus on relaxing the muscles in each area until they go limp.
Another technique: Imagining a calm scene, such as a babbling brook, and hearing the sound of it and the scent of the surrounding grass, can also bring relaxation.
These kinds of techniques occasionally come in handy for Wells, the senior in Oregon. Even though he’s O.K. much of the time, there’s still some lingering anxiety lurking below the surface. “Before I go to see one of my doctors, or the dentist, or even an eye doctor, I can feel the anxiety building in me,” he says. “Sometimes I use the techniques I learned. I do a breathing exercise and think, ‘Wait a minute, Jay, this is nothing. Just calm down.’”
“}]]
Support groups and meeting with a therapist can help.
Uncategorized, freelance, healthscienceclimate
Health – TIME
Support groups and meeting with a therapist can help.
Read moreEnglish News: How to Start Foraging, According to TikTokers
English News: How to Start Foraging, According to TikTokers
[[{“value”:”
There are more than 400,000 species of plants on Earth and at least half are suitable for human consumption—yet you’ll only find a small portion at the grocery store.
That’s part of the reason why Sam Thayer loves foraging. He started collecting wild food from the woods when he was a kid, and he still has cravings for delicacies he can’t buy. “Last year I gathered about 30 gallons of serviceberries”—blueberry-like fruits that grow on trees and shrubs—“and I make fruit leather and eat it as a snack year-round,” says Thayer, a naturalist who lives in Northwest Wisconsin and has authored an array of field guides. “I have about 8 pounds of Wapato, which is a tuber, in my pantry, and I grind it up into hot cereal for breakfast. I love it, and you can’t buy it.”
[time-brightcove not-tgx=”true”]
Foraging spiked in popularity during the pandemic, when people who felt unsafe going to the store discovered it was a fun way to collect healthy, nutrient-packed food from the great outdoors for free. It’s possible to forage in all sorts of places, even cities: Thayer recalls an excellent salad he made out of leaves plucked from trees in Washington, D.C. For all these reasons, foragers have found a home on TikTok, where millions of people watch videos explaining how to harvest puffball mushrooms, gather and process black walnuts, and make wild violet syrup.
We asked a few of TikTok’s most popular foragers, including Thayer (aka Well Fed Wild on TikTok), to share their best tips on getting started.
Do your homework before setting out
It’s often easiest to get a feel for foraging in your backyard or at a local park. But make sure to check the rules first: Some parks, nature centers, and other public properties don’t allow foraging, says Gabrielle Cerberville—aka “Chaotic Forager” on TikTok—who’s based in Charlottesville, Va. To find out, check an online resource like your state’s Department of Natural Resources, or contact someone from the park you’re interested in foraging at, she advises.
Read More: 7 Ways to Bring a Dead Friendship Back to Life
It’s also best not to forage where there’s obvious pollution, like near train tracks or next to busy highways. And while perhaps it should go without saying, don’t forage on private property unless you have explicit permission. Alexis Nikole Nelson—aka the “Black Forager” on TikTok—sometimes passes homes in her neighborhood in Columbus, Ohio, with super unusual or eclectic plants. She leaves a note with her contact information, which “puts the ball in their court,” she says. “When I see a yard and I’m like, ‘Oh my God, three pawpaw trees and a persimmon,’ I know I need to become their friend.”
Stock up on simple supplies
You don’t need much gear to forage, experts agree. Nelson likes to take a swiss army knife, which she might use to saw a branch that’s fallen across a trail or to cut a mushroom off a tree. She wears a backpack filled with cotton satchels that she can put her finds in to keep them separate and organized until she gets home; plastic grocery store bags also do the trick. As for what to wear? “I would love to say that I’m always in nice, sturdy hiking boots, but I find myself foraging in platform Crocs more frequently,” she says with a laugh. Closed-toe shoes are always a good idea when you’re venturing out in nature.
Look for easy-to-identify fruits and veggies
If you’re new to foraging, look for what you already know, Cerberville advises—like dandelions. You can do a lot with the easy-to-spot flowers: “Every part is edible,” she says. “The roots can be roasted and brewed, kind of like coffee. They’re also really good ground up and put into coffee cake or different sorts of baked goods.”
Read More: What to Know About Orienteering, the ‘Thinking Sport’
Flowers like lilacs and roses, meanwhile, can be turned into a simple syrup that looks and tastes like honey, Cerberville says. Or, you can add them to a salad for a splash of color. You might also recognize field garlic, a common weed that can be used as a substitute for garlic or onion powder. To figure out what’s in season near you, join local foraging groups on Facebook. Members tend to post photos of their daily finds, which can inspire your search.
Only eat something if you’re positive you know what it is
A rule of thumb: Don’t put something in your mouth if you can’t identify it with 100% confidence. If you’re uncertain, check your field guide, Thayer recommends. When a forager eats something they shouldn’t, it usually stems from carelessness, not misidentification, Thayer says—someone shoves a weed or mushroom into their mouth, for instance, without attempting to figure out what it is.
Don’t over-complicate your recipes
People tend to relish the scavenger-hunt aspect of foraging—but once they get home, they aren’t sure what to do with their finds, Nelson says. Some feel like their entire dish needs to be foraged, a TikTok-worthy concoction that wouldn’t be found in any cookbooks. Take the pressure off, she advises, and consider which foraged ingredients could stand in for ones you already love.
Nelson enjoys spinach and artichoke dip, for example, so she now makes it out of foraged lamb’s quarters (wild spinach) and burdock (a root vegetable). And instead of blueberry muffins, she makes serviceberry muffins. “You don’t have to rebuild the wheel,” she says.
Be respectful
Foragers tend to be ecologically conscious and committed to preserving and protecting the land. “We’re thinking sometimes years in advance about wanting to be able to come back to the same spot and enjoy the same bounty,” Cerberville says. It’s essential to be mindful of how you move through the environment, leaving no sign that you were there.
Read More: Put Your Shoes Back On. Here’s the Problem With Going Barefoot
Another rule of thumb: Take only what you need. This helps ensure the plant or fungi will continue to grow back—and that there will be some left for the other people and animals that pass by next. Take mushrooms, for example. “Deer eat mushrooms, squirrels eat mushrooms,” Cerberville notes. “It’s really important that when we’re talking about sustainability, we’re thinking not just in an anthropocentric way, but in an ecologically deep way where we’re considering the needs of everything around us.”
Have fun
People have different reasons for foraging: the food is healthy, it saves money. “But those are just the excuses we make up,” Thayer says. “The secret is, it’s fun.” He describes searching for and collecting wild food as awe-inspiring and gratifying. “It’s such a profound joy when you come across a lake where the wild rice is ripe, and you’re like, ‘We’re going to get our year’s supply of rice today,’” he says. He recalls a recent visit to a nearby farm where, with the owner’s permission, he picked 76 gallons of hickory nuts. He pressed them into cooking oil and gave bottles away to friends and family. “Foraging has the self-reliant joy of being connected to what it is to be human,” he says.
“}]]
Everything you need to know before making wild violet syrup or serviceberry muffins.
Uncategorized, Evergreen, healthscienceclimate
Health – TIME
Everything you need to know before making wild violet syrup or serviceberry muffins.
Read moreEnglish News: What to Know About Sports Betting and Problem Gambling Amid Ohtani Scrutiny
English News: What to Know About Sports Betting and Problem Gambling Amid Ohtani Scrutiny
[[{“value”:”
The firing of Los Angeles Dodgers star Shohei Ohtani’s interpreter and close friend after allegations of illegal gambling and theft from the Japanese baseball player is shining renewed attention on compulsive gambling.
The team fired interpreter Ippei Mizuhara, who has been Ohtani’s constant companion since the star came to the U.S in 2017, on Wednesday after reports about his alleged ties to an illegal bookmaker and debts well over $1 million.
[time-brightcove not-tgx=”true”]
The law firm representing Ohtani said in a statement that he had been the victim of “massive theft.”
Mizuhara told ESPN this week that Ohtani knew nothing of his illegal wagers on international soccer, the NBA, the NFL and college football. Mizuhara said Ohtani was an innocent victim of his friend’s gambling addiction.
What is problem gambling?
The National Council on Problem Gambling defines gambling addiction as “gambling behavior that is damaging to a person or their family, often disrupting their daily life and career.”
Gambling addiction is a recognized mental health diagnosis, and the group says anyone who gambles can be at risk for developing a problem.
Its symptoms include thinking about gambling all the time; feeling the need to bet more money more often; going back to try to win money back, known as “chasing losses;” feeling out of control; and continuing to gamble despite negative consequences.
How widespread is it?
The council says about 2.5 million adults in the U.S. meet the criteria of having a severe gambling problem. Another 5 million to 8 million people are considered to have mild or moderate gambling problems.
The 800-GAMBLER hotline can offer help and referrals, and Gamblers Anonymous also has resources and support for those with a gambling problem.
Where is sports betting legal?
Sports betting is legal in 38 U.S. states plus Washington, D.C., since a 2018 U.S. Supreme Court ruling that opened the floodgates to legal wagering in a case brought by New Jersey. More than 80% of sports betting is done online, using phones or laptops.
On Thursday, at the start of the NCAA college basketball tournament, the American Gaming Association estimated that Americans would wager $2.72 billion with legal outlets this year on the tournament.
What are sports leagues doing about gambling?
Major professional sports leagues prohibit their players from gambling, and many impose penalties including fines, suspensions and lifetime bans for violations.
The most famous of these involves baseball star Pete Rose, the sport’s all-time hits leader, who was banned for betting on games in which his team was involved.
Baseball’s collective bargaining agreement includes an annual spring training education program for players on safety and security, including issues relating to sports betting and gambling.
This comes at the same time that the leagues—who bitterly fought against legalizing sports betting beyond the four states that allowed in before 2018—have become business partners with the biggest gambling outlets. Many teams and league have official sports betting partners and allow gambling company advertising on their premises. A few have even opened sports books at their stadiums.
Is betting legal in California or Japan?
Sports betting is not legal in California, despite several attempts to have voters legalize it. In Japan, most forms of gambling are prohibited, although it is allowed on horse racing, motor sports and public races involving bicycles, power boats and motorcycles.
“}]]
Major professional sports leagues prohibit players from gambling even as they have become business partners with big betting outlets.
Uncategorized, News Desk, overnight, wire
Health – TIME
Major professional sports leagues prohibit players from gambling even as they have become business partners with big betting outlets.
Read moreEnglish News: A Man Has Received the First Pig-Kidney Transplant
English News: A Man Has Received the First Pig-Kidney Transplant
[[{“value”:”
The first reported person in the world has received a genetically modified pig kidney. A transplant surgeon at Massachusetts General Hospital successfully performed the groundbreaking, four-hour procedure on Richard Slayman, a 62-year-old manager at the Massachusetts Department of Transportation, on March 16. His doctors report he is doing well and expect him to leave the hospital soon.
The surgery was the culmination of years of work transplanting kidneys from a specially bred group of pigs—which had been genetically modified to more closely resemble those of humans—into primates. Encouraged by those results, the team at Mass General Brigham—the health system to which the hospital belongs—was confident it was time to test the pig organs in the first patient.
Slayman had received a human kidney transplant five years ago, but like so many people with kidney disease, the organ began to fail and he continued to need dialysis. Even those frequent efforts to replenish his kidney function weren’t enough, however, and his health progressively worsened. “At one point, he literally said, I just cannot go on like this,” said Dr. Winfred Williams, Slayman’s physician and associate chair of nephrology at Massachusetts General Hospital, during a March 21 briefing.
Dr. Tatsuo Kawai, director of the Massachusetts General Hospital’s Legorreta Center for Clinical Transplant Tolerance, was Slayman’s kidney transplant surgeon five years ago, and he also performed the pig-kidney surgery. While more than a dozen people in the operating room watched, Kawai carefully connected the pig kidney to Slayman’s circulatory system—not an easy task, given the patient’s history of diabetes and hypertension, which had weakened his blood vessels. “The size of the pig kidney was exactly the same as the human kidney,” Kawai said during the briefing. “Upon restoration of blood flow into the kidney, the kidney pinked up immediately and started to make urine. When we saw the first urine output, everyone in the operating room burst into applause. It was truly the most beautiful kidney I have ever seen.”
The pig donor
The kidney came from a special group of pigs bred to produce human-like kidneys. eGenesis, a biotech company that has been studying ways to make animal tissues as human as possible, worked closely with the research team at Mass General Brigham to come up with the right genetic animal donors that would make their organs safe enough to transplant into people, and effective enough to take over their kidney function.
Several genetic innovations over the past few decades made such a feat possible. The pigs’ cells were treated with the gene-editing technology CRISPR, which allows scientists to make very precise genetic changes in cells. These CRISPR-ed cells were then used to create pig clones so the pigs would have identical and consistent genetic changes. Their kidneys were then transplanted first into primates, and finally into Slayman.
All told, the pig kidneys contained 69 genetic changes in three major categories. The scientists knocked out or eliminated three pig genes that trigger immediate rejection by the human immune system, added seven human genes to make the pig tissue appear more human to the immune cells, and inactivated viral genes in pig cells that could cause infections. They also used a unique cocktail of antibody treatments to further dampen the immune reaction and give the transplanted kidney the best chance of surviving in the patient.
Next steps
eGenesis is working on other pig organs as well. In January, the company partnered with researchers at the University of Pennsylvania to transplant a genetically modified pig liver into a brain-dead patient. That work, along with Slayman’s experience, is making a strong case for the role of pig organs in addressing the shortage of organs for thousands of patients on waiting lists. More than 100,000 people are placed on the kidney transplant waiting list in the U.S. each year, while only 20,000 kidneys are available.
The Mass General Brigham team hopes to perform more of these transplants to get a better idea of how long the pig kidneys can function and whether they can meaningfully extend the length and quality of patients’ lives. For now, says Williams, patients on the waiting list or dialysis could potentially benefit from receiving a pig kidney temporarily as they wait for a human one. Even such bridging can be critical for patients like Slayman; while he had been on dialysis, he experienced clotting issues that compromised the blood flow required to make it effective and required dozens of surgeries to improve his circulation. Pig kidneys could become a realistic option for people like him for whom dialysis becomes too challenging.
The long-term hope is that pig kidneys may even become a substitute for human organs if they prove up to the task. “We never anticipated dialysis would become a lifelong solution for kidney failure,” said Dr. Leonardo Riella, medial director of kidney transplantation at Mass General Brigham and lead investigator of the trial. “Yet this is the stark reality for over 600,000 patients in the U.S.; dialysis has sadly become their last resort for managing their disease. Now picture a different narrative, one where healthy kidneys are readily available for transplantation. Today we are offering a glimmer of hope that may one day be possible for many more patients.”
“}]]
The Massachusetts man is doing well and is expected to leave the hospital soon.
Uncategorized, healthscienceclimate
Health – TIME
The Massachusetts man is doing well and is expected to leave the hospital soon.
Read moreEnglish News: The World’s Most Expensive Drug Is Now a $4.25 Million Gene Therapy
English News: The World’s Most Expensive Drug Is Now a $4.25 Million Gene Therapy
[[{“value”:”
A new gene therapy for an ultra-rare disease will have a wholesale cost of $4.25 million, making it the world’s most expensive drug.
The one-time treatment, Lenmeldy, won U.S. regulatory approval on Monday to correct the underlying cause of a hereditary condition called early-onset metachromatic leukodystrophy, or MLD.
MLD is a fatal disease in which infants sometimes start to lose the ability to walk and talk. Orchard Therapeutics said the drug’s price “reflects its clinical, economic and societal value” in a statement Wednesday.
[time-brightcove not-tgx=”true”]
Read More: FDA Approves First CRISPR Treatment in U.S.
The drug’s cost tops that of CSL Behring LLC’s Hemgenix, a one-time infusion for hemophilia priced at $3.5 million.
MLD affects about one in 100,000 live births, and fewer than 40 children a year in the U.S., according to Orchard.
The company focuses on developing gene therapies, which aim to correct the underlying genetic flaws that cause inherited diseases. It was recently acquired by the Japanese drugmaker Kyowa Kirin Co.
The field of gene therapy has sparked debate over its high prices. Pharma companies say they are justified because the treatments can potentially cure patients, generating savings for the health-care system over time and delivering other societal benefits.
Drugmakers also want to recover the cost of developing treatments that are often aimed at small populations, limiting their revenue potential. But pricing has raised concern about the strain it could put on insurers, particularly Medicaid, the health-insurance program for the poor.
“}]]
It’s a one-time treatment for children with a rare genetic disease.
Uncategorized, healthscienceclimate, wire
Health – TIME
It’s a one-time treatment for children with a rare genetic disease.
Read moreEnglish News: Doctors Urge Refrigerating Acne Creams to Reduce Carcinogen Risk
English News: Doctors Urge Refrigerating Acne Creams to Reduce Carcinogen Risk
[[{“value”:”
Some dermatologists are recommending that people refrigerate benzoyl peroxide products such as Proactiv and Clearasil after an independent lab found they were contaminated with the potent carcinogen benzene.
The American Acne & Rosacea Society said Wednesday that storing benzoyl peroxide creams, gels and washes at refrigerated temperatures could minimize the risk of benzene exposure. “Benzoyl peroxide has been a very important part of the treatment of many patients with acne and also some other skin diseases,” according to the group, which has about 6,000 members.
[time-brightcove not-tgx=”true”]
Read More: Why Does My Face Turn Red When I Exercise?
The testing lab Valisure filed a petition with the U.S. Food and Drug Administration on March 5 asking the agency to recall benzoyl peroxide acne treatments after finding high levels of benzene in the products, Bloomberg News has reported. Benzene levels increased when products underwent stability testing, including Proactiv’s 2.5% benzoyl peroxide cream, manufactured by Taro Pharmaceutical Industries Ltd., and 10% benzoyl peroxide cream from Reckitt Benckiser Group Plc’s Clearasil.
The findings came as a surprise given benzoyl peroxide has been used for five decades, AARS President James Del Rosso said in a statement. The group said more research is needed.
“We want to be sure that any guidance that is given and any decisions that are made are based as much as possible on solid scientific evidence,” Del Rosso said.
The FDA has said it would work to verify the accuracy of the data Valisure presented in its petition.
“}]]
Some dermatologists are recommending the move after an independent lab found contamination with cancer-causing benzene.
Uncategorized, bloomberg wire, healthscienceclimate, wire
Health – TIME
Some dermatologists are recommending the move after an independent lab found contamination with cancer-causing benzene.
Read moreEnglish News: I Used ChatGPT as My Personal Trainer. It Didn’t Go Well
English News: I Used ChatGPT as My Personal Trainer. It Didn’t Go Well
[[{“value”:”
I love running. I will happily jog for hours (and often do, during marathons). But ask me to perform a push-up, and I might cry. I truly detest strength training.
Unfortunately for me, it’s extremely good for you—and for runners who want to get faster. So I decided to add in two strength-training sessions per week in preparation for running the Boston Marathon this spring.
[time-brightcove not-tgx=”true”]
I wanted exercises designed to improve my pace, but didn’t want to spend money on a personal trainer. Unsure of how to start, I turned to ChatGPT.
The chatbot did not give me the workout regimen I was hoping for—and after following its recommendations for nearly a month, I was no closer to liking strength training. But I learned some things along the way that might end up helping me become a better runner.
Lesson 1: ChatGPT is not much of a coach
OpenAI’s free AI chatbot is trained on vast amounts of data from sources around the Internet so it can answer prompts with human-like text. To test out its workout recommendations, I first asked it to create a marathon training plan.
As a running coach who’s finished more than a dozen marathons, I have a good sense of what a solid training schedule looks like. The ChatGPT results were—not that. Although it told me to run about six days a week at various speeds and distances (so far, so good), it listed hill sprints and intervals without essential details like how fast or far. It also gave me no runs longer than 14 miles, aside from the suggestion to run a full marathon a week before the end—something no legitimate coach would ever advise, since that’s far too taxing on the body to be beneficial, especially so close to race day. I asked the question twice more, adding details about my fitness level and goals. Now, it only told me to run up to 12 miles. In comparison, the longest run on most respectable marathon plans is 18 to 22 miles.
Read More: Your Brain Doesn’t Want You to Exercise
It’s not hard to find a decent training plan online. So although I didn’t expect ChatGPT to invent a mindblowing regimen, I was surprised that the plans it spat out were so underwhelming and at times incomprehensible. But maybe I shouldn’t have been. What ChatGPT does so well is generate “a human-like, natural language output,” explains Richard Bayly, vice president of product, AI, and data at PEAR Health Labs, which owns the AI-powered fitness app Aaptiv. But while the chatbot is designed to sound like it knows what it’s talking about, it doesn’t.
ChatGPT’s primary skill lies in sounding human, not in giving expert recommendations. The website even include a disclaimer to “check your facts,” stating that the chatbot is not intended to give advice. Even so, people are already using the site for workout suggestions. (OpenAI didn’t respond to a request for comment for this piece.)
Lesson 2: ChatGPT generated decent exercise ideas
Although it failed my marathon plan litmus test, I still wanted to see if ChatGPT could give me some ideas for strength training. After asking “which body weight–only strength training exercises will help me run faster,” it listed 12 exercises that seemed fairly solid, hitting almost all the major muscle groups used in running. But as I started to do the workout, I realized I didn’t have any information on sets, reps, or whether I should do each exercise one at a time versus in a circuit.
I’m not the only one who has discovered ChatGPT’s workouts are missing fundamental details. One January 2024 study evaluating ChatGPT-generated workouts found its exercise recommendations were only 41% comprehensive—meaning its answers didn’t include all of the American College of Sports Medicine’s six components of exercise prescription: frequency, intensity, time, type, volume, and progression.
Read More: This Is the Best Time of Day to Work Out
Yet the researchers did find the workouts to be 90% accurate. Most of the inaccuracies involved telling people to get medical clearance to exercise when they didn’t need it. That might seem innocuous, but Linda Pescatello, a professor in the department of kinesiology at the University of Connecticut and one of the study’s authors, says this could discourage people from exercising altogether. “Requiring someone to get medical clearance is a major deterrent to undertaking an exercise program,” she says.
Done right, AI has real potential to get more of us moving. In a recent report funded by the sportswear company ASICS, 62% of women named the high cost of trainers as a major barrier to exercising. A free, easily accessible chatbot offering targeted, on-demand workout advice on a mass scale could be a boon to public health.
Lesson 3: The chatbot’s workouts are boring and uninspired
Two weeks into my strength-training plan, I found myself skipping certain moves and swapping in others instead. The problem was, I didn’t trust Coach ChatGPT. Did I really need to do burpees, or had the chatbot simply come across them in some random “workout for runners” article? The answers hadn’t given me any information on why I was doing the moves, or links to learn more, so I kept questioning the efficacy of the exercises.
Also, the workout was boring, made up of basic American gym-class exercises that felt cookie-cutter, despite all the personal info I’d included in my prompts.
“There’s the science of exercise prescription, and there’s the art,” says Pescatello. A robot might have completed my prescribed workout and gotten results, but I’m far too human to pump out the same 12 bland moves with gusto—especially without a trainer to hold me to it. “It doesn’t account for humanity at all,” says Kristie Larson, a New York–based personal trainer. “Sure, it might write a very good training plan—if you were also a machine.”
Lesson 4: Turn to a human if you get injured
At one point, my sartorius muscle in my thigh started to act up. I asked ChatGPT, “Can I still run if my sartorius muscle hurts?” It gave me a vague, long-winded answer that wasn’t exactly “no,” but suggested I stick to low-impact activities like walking if the “pain is mild and improving.”
I brought this up with New York-based adidas running coach Jessica Zapotechne. Was this sound or overly conservative advice? “That question makes me think about a topic that I talk with athletes about a lot, which is distinguishing between pain and discomfort,” she tells me. There are different types of hurting, and determining what is simply part of training versus signs of an injury requires “a list of questions to go through,” she says. That’s another problem with AI coaches: They don’t ask questions, the way a human coach typically would.
Read More: Should I Use a Foam Roller?
“You’ve got to be very careful about your inputs, because if you have bad inputs, you’re going to have bad outputs,” says Bayly of PEAR Health Labs. “A generative AI chatbot is relying largely on information that’s widely available. I don’t think there’d be a lot of difference between a generic program that you might be able to download off the Internet versus something the chatbot might return if you are not specific enough.” AI-based workout apps like Aaptiv have users answer several questions about their goals, experience, age, and more upfront in order to generate personalized recommendations, which are then refined further by tracking what the user does on the app, à la Netflix.
The trouble is, someone who’s looking to AI for exercise ideas probably doesn’t know exactly what details they’d need to share to get the most helpful answer.
“The person who has the skill to write a great command probably has enough skill to just write the workout,” says Chicago-based strength coach Elisabeth Akinwale. On the other hand, she adds, if someone is asking ChatGPT for workout help, they might not have the knowledge to realize when it spits out something wacky, like my marathon training plans. “They don’t have the discernment to say, no, that doesn’t sound right,” she says.
So what is ChatGPT good for, in the world of fitness?
In a word: “Variety,” says Pescatello. “One of the capabilities AI has in any profession is it can be a great search tool. With careful prompting, you could specify your preferences and an output could be generated that gives you more options than you feel there are now.” Larson echoes that sentiment, saying it would be best used by someone experienced who’s just looking to mix things up with a new idea to add to their rotation.
Still, you’d have to fit within a narrow population to get the best results. Pescatello says her team found that ChatGPT’s recommendations are currently biased toward adults and lack cultural awareness or considerations for disabilities. Their analysis also scored the readability at the college level.
Read More: The 3 Most Effective Exercise Moves That Don’t Require Equipment
Despite ChatGPT not turning out to be the free personal trainer I wanted, I’m still doing some of its recommended strength-training exercises regularly. I haven’t gotten faster yet, though we’ll see what happens on marathon day.
I find I keep going back to ask ChatGPT my 3 a.m. workout questions that feel too silly or inconsequential to bother another human with. It’s proven most useful after a session talking to a sports dietitian, when I needed a simple explanation of “anabolic potential.” The first few results Google brought up were too sciencey, but when I asked ChatGPT to define it for an eighth grader, I got exactly what I was looking for: “the body’s ability to build and repair tissue, especially muscles.” I’m finally using it for what it’s designed to do: not to give exercise advice, but to generate natural-sounding, easy-to-understand language.
“}]]
The chatbot did not give me the workout regimen I was hoping for.
Uncategorized, Evergreen, freelance, healthscienceclimate
Health – TIME
The chatbot did not give me the workout regimen I was hoping for.
Read more